Mpox

If you think you have been exposed to mpox, call your healthcare provider for more information. Healthcare providers can refer to Mpox Healthcare Provider Information (mt.gov) for additional information. For more information on the U.S. mpox situation, visit CDC's webpage.
What You Need to Know
Mpox is a viral infection transmitted through close, personal contact, including kissing, sex, and other skin-to-skin or face-to-face contact. Most infections last 2-4 weeks and resolve without specific treatment. The type of mpox seen in this outbreak is rarely fatal, and more than 99% of people who get this form of the disease are likely to survive.
The data current show transmission is higher among people in close social networks. Men who have sex with men have been disproportionately impacted by this outbreak, but anyone who has been in close, personal contact with someone who has mpox is at risk. People with mpox in the current outbreak generally report having close, sustained physical contact with other people who have mpox.
Key Symptoms:
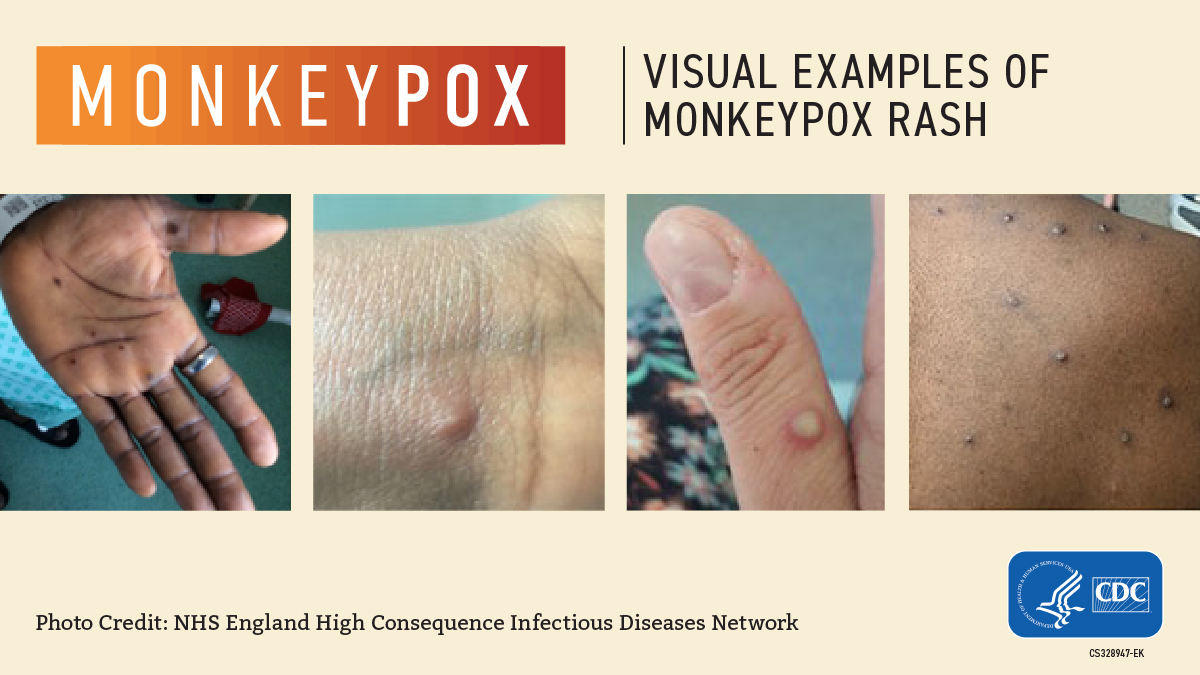
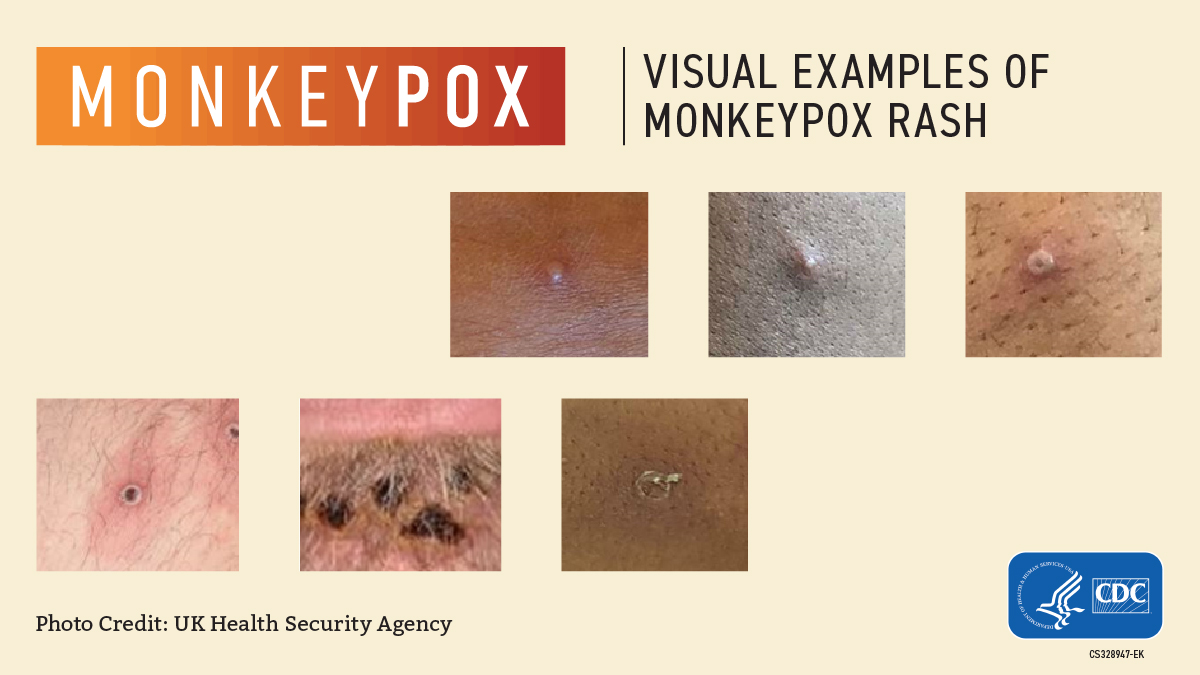
A Rash, Bumps, or Blisters that may be located on or near the genitals or anus but could also be on other areas like the hands, feet, chest, face, or mouth.
- The rash will go through several stages, including scabs, before healing.
- The rash can look like pimples or blisters and may be painful or itchy.
- The rash may look similar to syphilis, herpes, or other common skin rashes.
Other Symptoms:
- Fever & headaches
- Muscle aches
- Swollen lymph nodes
- Chills
- Exhaustion
- Respiratory symptoms
Symptom onset ranges from 5-21 days after exposure to the virus
- Avoid close contact, including sex or being intimate with anyone, until you have been checked out by a healthcare provider.
- When you see a healthcare provider, wear a mask.
CDC provides recommendation for non-hospitalized patient infection prevention measures in their document, Isolation and Infection Control
Get Both Doses of the Mpox Vaccine
Mpox vaccination is not recommended for the general public, but it is recommended for those at increased risk for infection or at increased risk for developing severe disease. Vaccination is available in Montana for people who self-identify as being at increased risk for infection. There is no requirement to specify a reason beyond a self-attestation at the time of vaccination.
Below are some examples of individuals that may be at increased risk.
- Adults 18 years* and older who meet one of the following criteria:
- Individuals who have recently had multiple or anonymous sexual partners; OR
- Partners of individuals who have recently had multiple or anonymous sexual partners; OR
- Sex workers; OR
- Staff at establishments where sexual activity occurs (e.g., bathhouses, saunas, sex clubs); OR
- Were diagnosed with gonorrhea or early syphilis within the past 12 months; OR
- Persons experiencing homelessness with high-risk behaviors; OR
- Are on HIV pre-exposure prophylaxis; OR
- Are part of high risk cohorts identified by clinical staff in the correctional system; OR
- Individuals deemed to be high-risk based on individual risk assessments
Persons who meet the criteria above and are immunocompromised or those who have underlying medical conditions that confer increased risk for severe disease (e.g., atopic dermatitis, eczema, HIV) should be prioritized for vaccination.
Post- Exposure Prophylaxis (PEP):
- Adults 18+ years and older who have had an exposure to a(n) individual(s) with confirmed orthopoxvirus / mpox virus infection.
FAQS
Anyone can get mpox, but some people are at a higher risk. Unlike the virus that causes COVID-19, monkeypox does not spread easily between people. Mpox is primarily spread through close contact and does not spread through the air over longer distances. Brief interactions that do not involve physical contact and health care interactions conducted using appropriate protective equipment are generally considered low risk.
While the current cases nationally and internationally mainly involve men who have sex with men, anyone who is sexually active with multiple partners or who are partners with someone who has sex with multiple partners can be at risk for being exposed to mpox.
Other risk factors may include travel to areas where mpox is spreading, close, non-sexual contact with a known case, or contact with sick animals. To protect yourself and others from mpox or sexual infectious diseases, DPHHS recommends practicing safe sex methods, practice harm reductions, and avoiding sexual contact with anyone who has open wounds, sores, or rashes
- See a healthcare provider if you notice a new or unexplained rash or other mpox symptoms.
- Remind the healthcare provider that mpox is circulating.
- Avoid close contact (including intimate physical contact) with others until a healthcare provider examines you.
- Avoid close contact with pets or other animals until a healthcare provider examines you.
- If you’re waiting for test results, follow the same precautions.
- If your test result is positive, stay isolated and observe other prevention practices until your rash has healed, all scabs have fallen off, and a fresh layer of intact skin has formed.
- Remain isolated if you have a fever or respiratory symptoms, including sore throat, nasal congestion, or cough. Only go out to see a healthcare provider or for an emergency and avoid public transportation.
- If you need to leave isolation, you should cover the rash and wear a well-fitting mask.
Mpox spreads in different ways. The virus can spread from person-to-person through direct contact with the infectious rash, scabs, or body fluids. It also can be spread by respiratory secretions during prolonged, face-to-face contact, or during intimate physical contact, such as kissing, cuddling, or sex. In addition, pregnant people can spread the virus to their fetus through the placenta.
Touching items (such as clothing or linens) that previously touched the infectious rash or body fluids is another way monkeypox spreads. It’s also possible for people to get mpox from infected animals, either by being scratched or bitten by the animal or by eating meat or using products from an infected animal.
People who do not have mpox symptoms cannot spread the virus to others.
Mpox can spread from the time symptoms start until the rash has fully healed and a fresh layer of skin has formed. The illness typically lasts 2-4 weeks.
People with mpox should avoid contact with animals, including pets, domestic animals, and wildlife to prevent spreading the virus.
During the 2003 mpox outbreak in the United States, we did not see disease spread to domestic animals other than prairie dogs, and we do not have reason to believe that we will see that now. However, we still recommend that people with mpox avoid interacting with animals and find someone else to take care of their pets while they recover.
Evidence of human-to-dog transmission of monkeypox virus - ScienceDirect
Many mpox infections last 2 to 4 weeks and resolve without treatment. There are no treatments specifically for mpox virus infections. However, because of genetic similarities in the viruses, antiviral drugs used to treat smallpox may be used to treat mpox infections. The need for treatment will depend on how sick someone gets, where lesions are located, and whether they are likely to get severely ill, including individuals with weakened immune systems. Please consult a healthcare provider for more information.
There are two types of mpox virus - Clade I and Clade II Infections in the current outbreak are from the West African type. The Clade I strain has a fatality rate around 10%. This strain is not associated with the current outbreak.
Infections with the type of mpox virus identified in the 2022 outbreak—the Clade IIb type—are rarely fatal.
- More than 99% of people who get this form of the disease are likely to survive. However, people with severely weakened immune systems, children under 1 year of age, people with a history of eczema, and people who are pregnant or breastfeeding may be more likely to get seriously ill or die.
- Although the clade II type is rarely fatal, symptoms can be extremely painful, and people might have permanent scarring resulting from the rash.
- In this current outbreak, 42 people in the US have died of mpox.
Young children (<1 year of age), individuals who are pregnant or have weakened immune systems, and people who have a history of certain skin conditions (e.g., eczema) may be at increased risk for severe infections.
We encourage anyone who has a rash and thinks they may have had close, skin-to-skin contact with someone who could have mpox in the last 21 days to talk to their medical provider and find out if they should be tested.
Vaccination with Jynneos is recommended for individuals who at high risk for infection to prevent mpox. Jynneos vaccine is licensed as a two-dose series administered 28 days (4 weeks) apart.
Jynneos can be administered using either the standard regimen which involves a subcutaneous injection of 0.5mL, or the alternative regimen which involves an intradermal injection of 0.1mL. The standard regimen is the FDA-approved dosing regimen for individuals 18+. The alternative regimen is authorized under an Emergency use Authorization since August 9, 2022 for individuals 18+. The August 9, 2022 Emergency Use Authorization also authorized the standard regimen for people aged <18.
Vaccination is available in Montana to people who self-identify as being at increased risk for infection. There is no requirement to specify a reason beyond self-attestation at the time of vaccination.
Below are some examples of individuals that may be at increased risk.
Pre-exposure prophylaxis (PREP):
- Adults 18* and older who meet one of the following criteria:
- Individuals who have recently had multiple or anonymous sexual partners; OR
- Partners of individuals who have had multiple or anonymous sexual partners; OR
- Sex workers; OR
- Staff at establishments where sexual activity occurs (e.g., bathhouses, saunas, sex clubs); OR
- Were diagnosed with gonorrhea or early syphilis within the past 12 months; OR
- Persons experiencing homelessness with high-risk behaviors; OR
- Are on HIV pre-exposure prophylaxis; OR
- Are part of high risk cohorts identified by clinical staff in the correctional system; OR
- Individuals deemed to have high-risk based on individual risk assessments.
Post-exposure prophylaxis (PEP):
- Adults 18 years* and older who have had exposure to individuals with confirmed orthopoxvirus/monkeypox virus infection.
Post-exposure prophylaxis ++ (PEP++):
- Adults 18 years* and older who have had multiple sexual partners in the past 14 days in a jurisdiction with known monkeypox
- This may include:
- Known contacts who are identified by public health via case investigation, contact tracing, and risk exposure assessments
- People who are aware that one of their sexual partners from the past 2 weeks has received a monkeypox diagnosis.
- Gay, bisexual, other men who have sex with men, and transgender people who report any of the following in the past 2 weeks:
- Group sex or sex with multiple partners.
- Sex at a commercial sex venue or in association with an event, venue, or defined geographic area where monkeypox transmission has been reported.
Note: eligible persons, per the criteria above, who are immunocompromised (e.g., those with advanced or uncontrolled HIV) or those who have underlying medical conditions that confer increased risk for severe disease (e.g., atopic dermatitis, eczema) could be prioritized for vaccination.
- Certain healthcare and public health response team members designated by public health authorities to be vaccinated for preparedness purposes according to ACIP guidance.
At this time, most clinicians in the U.S. and laboratorians not performing the orthopox generic test to diagnose orthopoxviruses, including Monkeypox virus, are not advised to receive monkeypox vaccine PrEP
*For individuals under the age of 18 years, Jynneos may be administered under the current EUA as a 2-dose 0.5 mL subcutaneous injection given 28 days apart.
Vaccine is located at several locations throughout Montana. Please visit Monkeypox Vaccine Locator · Monkeypox Vaccine Locator (mpoxvaxmap.org) to find a mpox vaccine provider. If there is not a provider in your area, please contact your local health department to coordinate vaccination
Please contact your healthcare provider or your local health department to know if you're eligible for vaccination.