Guidance for Certifying COVID-19 Deaths
It is important to emphasize that Coronavirus Disease 2019 or COVID-19 should be reported on the death certificate for all decedents where the disease caused or is assumed to have caused or contributed to death. An accurate count of the number of deaths due to COVID–19 infection, which depends in part on proper death certification, is critical to ongoing public health surveillance and response. When a death is due to COVID–19, it is likely the Underlying Cause of Death and thus, it should be reported on the lowest line used in Part I of the death certificate. Ideally, testing for COVID–19 should be conducted, but it is acceptable to report COVID–19 on a death certificate without this confirmation if the circumstances are compelling within a reasonable degree of certainty. For all other deaths where a different coronavirus was involved, please include the viral subtype in the cause of death section (i.e. Coronavirus OC43). This will help distinguish between the novel pandemic virus and other circulating strains while reducing the need for vital statistics staff to contact certifiers to determine this information.
Resources
1. Finalized Written Guidance.
2. Video Guidance for Certifying COVID-19 deaths.
4. General Guidance on Death Certification.
1. Finalized Written Guidance.
The National Center for Health Statistics has released its finalized Guidance for Certifying Deaths to Coronavirus Disease 2019 (COVID-19). The updated guidelines include the example described below plus additional scenarios on certifying deaths in the presence of co-morbidities and in the absence of COVID-19 testing.
2. Video Guidance for Certifying COVID-19 deaths.
To supplement the published guidance on filling out death certificates for deaths related to COVID-19, the National Center for Health Statistics (NCHS) has released a short video on the NCHS YouTube channel. The video runs a little over 3 minutes and can be accessed directly at https://youtu.be/oL3VMwieAms.
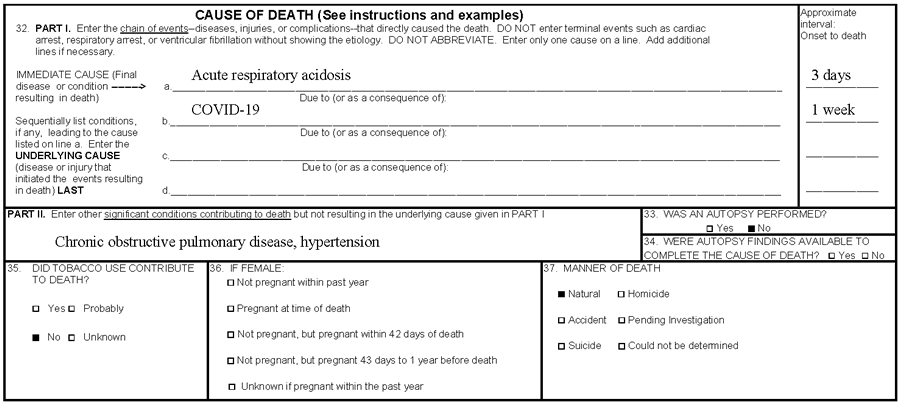
Scenario I: A 77-year-old male with a history of hypertension and chronic obstructive pulmonary disease
A 77-year-old male with a 10-year history of hypertension and chronic obstructive pulmonary disease (COPD) presented to a local emergency department complaining of 4 days of fever, cough, and increasing shortness of breath. He reported recent exposure to a neighbor with flu-like symptoms. He stated that his wheezing was not improving with his usual bronchodilator therapy. Upon examination, he was febrile, hypoxic, and in moderate respiratory distress. His chest x-ray demonstrated hyperinflation and his arterial blood gas was consistent with severe respiratory acidosis. Testing of respiratory specimens indicated COVID–19. He was admitted to the ICU and despite aggressive treatment, he developed worsening respiratory acidosis and sustained a cardiac arrest on day 3 of admission.
Comment: In this case, the acute respiratory acidosis was the immediate cause of death, so it was reported on line a. Acute respiratory acidosis was precipitated by the COVID–19 infection, which was reported below it on line b. in Part I. The COPD and hypertension were contributing causes but were not a part of the causal sequence in Part I, so those conditions were reported in Part II.
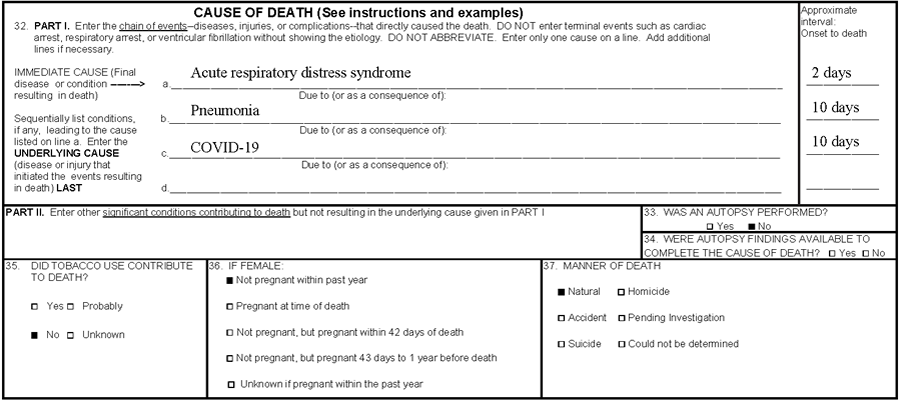
Scenario II: A 34-year-old female with no significant past medical history
A 34-year-old female with no significant past medical history presented to her primary care physician complaining of 6 days of fever, cough, and myalgias. She was found to be febrile, hypotensive, and hypoxic. She was admitted to the hospital and underwent a CT scan of the chest, which revealed diffuse ground-glass opacification indicative of viral pneumonia. Respiratory specimens were sent for testing and rRT-PCR confirmed COVID–19. Her condition deteriorated over the next 2 days and she developed acute respiratory distress syndrome (ARDS). She was transferred to the ICU and started on positive pressure ventilation. Despite aggressive resuscitation, the patient expired on hospital day 4.
Comment: In this case, the immediate cause of death was ARDS, so it was reported on line a. as a consequence of pneumonia, which was reported on line b. The underlying cause of death (UCOD) was COVID–19 so it was reported on line c., the lowest line used in Part I.
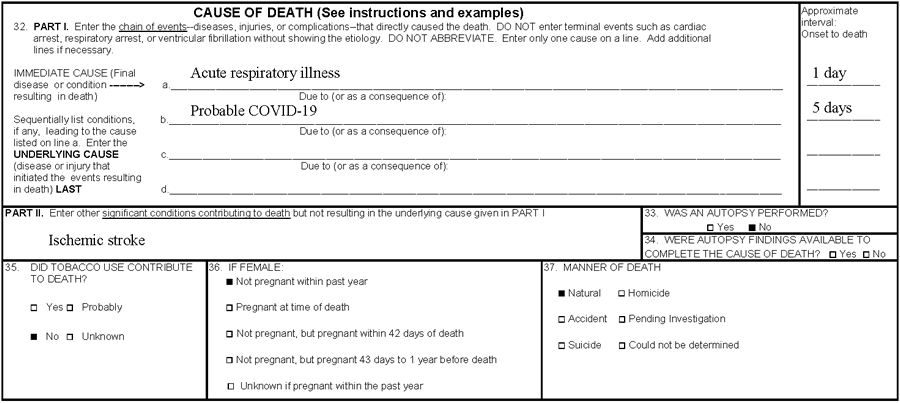
Scenario III: An 86-year-old female with an unconfirmed case of COVID–19.
An 86-year-old female passed away at home. Her husband reported that she was nonambulatory after suffering an ischemic stroke 3 years ago. He stated that 5 days prior, she developed a high fever and severe cough after being exposed to an ill family member who subsequently was diagnosed with COVID–19. Despite his urging, she refused to go to the hospital, even when her breathing became more labored and temperature escalated. She was unresponsive that morning and her husband phoned emergency medical services (EMS). Upon EMS arrival, the patient was pulseless and apneic. Her husband stated that he and his wife had advanced directives and that she was not to be resuscitated. After consulting with medical command, she was pronounced dead and the coroner was notified.
Comment: Although no testing was done, the coroner determined that the likely UCOD was COVID–19 given the patient’s symptoms and exposure to an infected individual. Therefore, COVID–19 was reported on the lowest line used in Part I. Her ischemic stroke was considered a factor that contributed to her death but was not a part of the direct causal sequence in Part I, so it was reported in Part II.
4. General Guidance on Death Certification.
For more general guidance and training on cause-of-death reporting, certifiers can be referred to the Cause of Death mobile app available through https://www.cdc.gov/nchs/nvss/mobile-app.htm [cdc.gov] and the Improving Cause of Death Reporting online training module, which can be found at https://www.cdc.gov/nchs/nvss/improving_cause_of_death_reporting.htm [cdc.gov].

