Rabies

What You Need to Know
Rabies is a preventable viral disease of humans and mammals most often transmitted through the bite of a rabid animal. The vast majority of rabies cases reported each year occur in wild animals like raccoons, skunks, bats, and foxes. The US averages 1-3 deaths per year reported due to rabies.
Rabies virus is transmitted through direct contact (such as through broken skin or mucous membranes in the eyes, nose, or mouth) with saliva or brain/nervous system tissue from an infected animal.
People usually get rabies from the bite of a rabid animal. It is also possible, but rare, for people to get rabies from non-bite exposures, which can include scratches, abrasions, or open wounds that are exposed to saliva or other potentially infectious material from a rabid animal. Other types of contact, such as petting a rabid animal or contact with the blood, urine or feces of a rabid animal, are not associated with risk for infection and are not considered to be exposures of concern for rabies.
Potential Exposure to Rabies
Wild Animals Rabies Surveillance in the United States 2013-2017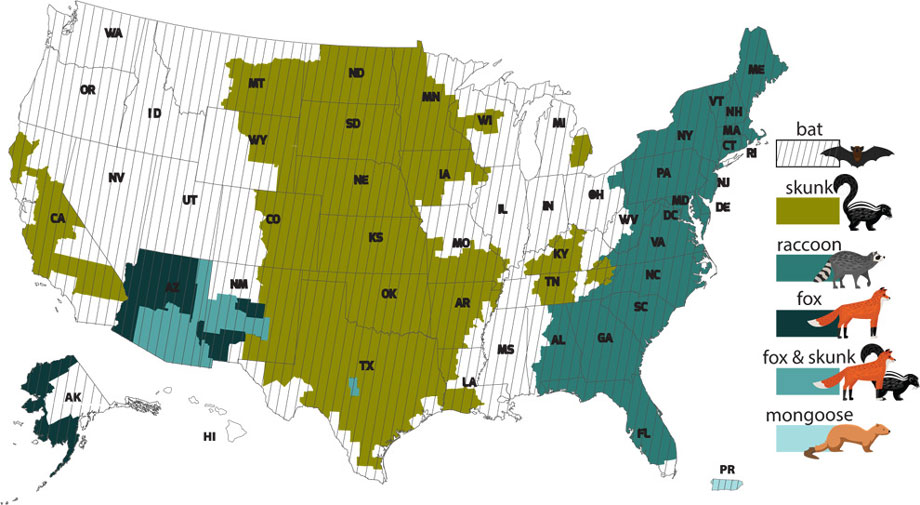
When potential exposures to rabies occur, consultation with your healthcare provider or local public health jurisdiction is recommended. Preventative treatment, known as rabies post-exposure prophylaxis (rPEP), is administered to prevent the development of disease. Please see the table below for information regarding exposures by various animal species. International exposures to rabies require further assessment by public health. To contact your local health department, please visit the DPHHS website for local public health office contact information.
Potential exposure to rabies:
| Bites | Bites that break the skin from an animal capable of transmitting the rabies virus are a potential rabies exposure. Bites from cats and dogs are the most commonly reported exposures from pets in MT. |
| Bat Exposures |
Most bats are not rabid. However, any direct contact between a human and a bat should be evaluated for an exposure. Other situations that might qualify as exposures
include finding a bat in the same room as a person who might
be unaware that a bite or direct contact had occurred, such as those who are sleeping.
|
| Non-Bite Exposures |
This type of exposure rarely causes rabies. The contamination of open wounds or abrasions (including scratches) or mucous membranes with saliva or other
potentially infectious material, like brain matter, from a
rabid animal also constitutes a non-bite exposure.
|
| Do you think you were potentially exposed? | Contact your local healthcare provider or local health department |
|
The following is not considered a potential exposure to rabies:
|
|
Contact your local health department, local public health office contact information and/or call a healthcare provider.
The rabies virus infects the central nervous system and is almost universally fatal in humans. The virus is slow moving, so there is time to perform animal assessments after a potential exposure. According to CDC, no person in the United States has ever contracted rabies from a dog, cat, or ferret that was confined and observed for 10 days.
Are you from a state other than Montana and have questions? Please see the CDC website listing state and local rabies consultation contacts. Management of potential rabies exposures may differ depending on the location, so it is important to consult with your local health contacts.Rabies in a human or animal, or exposure to a human by a species susceptible to rabies infection is a reportable condition to the local health departments in the state of Montana (ARM 37.114.203).
| Animal Type | Evaluation and Disposition of the Animal |
Rabies Post Exposure Prophylaxis (rPEP) Recommendations |
| Dogs, Cats, and Ferrets |
Healthy and available for 10 day observation |
Do not seek or administer rPEP initially. Contact public health to evaluate the exposure and, if possible, arrange for safe observation or assessment of the animal. Administer rPEP if determined to have rabies during the observation period. |
| Dogs, Cats, and Ferrets |
Animal available but has signs or symptoms suggestive of rabies |
Contact public health, and an assessment by veterinarian is required. Seek or administer rPEP if public health determines the animal is rabid, or rabies cannot be ruled out. |
| Dogs, Cats, and Ferrets |
Unknown, unable to locate the animal |
Case by case assessment with local public health. Seek or administer rPEP if recommended by local public health. |
| Bats and Skunks | High risk animal for rabies in MT, regard as rabid unless animal testing proves it is not rabid |
Contact local public health to report exposure and for assistance with animal testing. Seek or administer rPEP if animal unavailable for testing, or if testing is indeterminate, and notify local public health of the administration. |
| Wild mammalian animals (except lagomorphs and small rodents) |
Medium risk for animal rabies in MT, regard as rabid unless animal testing is negative |
Contact local public health to report exposure, and for assistance with animal testing. Public health may recommend rPEP. |
| Livestock (horses, pigs, cattle and other large animal species) |
Low risk for rabies in Montana |
Case by case assessment with local public health. Public health may recommend administration of rPEP. |
| Domesticated and Wild Animal Species that are not a Rabies Concern in MT* |
| All amphibian, All birds, All reptiles, Gopher, Mole, Squirrel, Guinea pig, Mouse, Vole, Hamster, Rabbit, Chipmunk, Hare, Rat, Gerbil, Hedgehog, Shrew |
Resources by Animal
- CDC website: Bats and rabies
- Bat Conservation International: Bats and rabies
- Contains information on how to safely capture bats
- Contains information regarding pet exposures to potentially rabid animals
- MT Department of Agriculture: Management of House Bats

