Montana Medicaid and Healthy Montana Kids (HMK) Plus
Montana Medicaid and HMK Plus are healthcare benefits for eligible low-income Montanans. Montana Medicaid and HMK Plus pays for services that are:
- Medically necessary,
- Provided by a Montana Medicaid/HMK Plus enrolled provider, and
- Medicaid/HMK Plus covered services.

The Montana Department of Health and Human Services (DPHHS) has extended coverage to postpartum women. This change will now allow postpartum women enrolled in Montana's Medicaid and Healthy Montana Kids Programs to be eligible for 12-month continuous coverage. If you are a member and become pregnant or have any changes to your pregnancy, notify the Office of Public Assistance (OPA). Providing the most updated information on your pregnancy or postpartum status will ensure you are covered under this extension. If OPA is not notified, they will be unable to change or extend your coverage. Women that have become pregnant or had changes to a pregnancy since July 1, 2023, must report these changes to OPA via:
- Self-service portal located at https://apply.mt.gov/
- Providing a written statement of the pregnancy or changes to the local OPA office
- Calling the Public Assistance Help Line at 1-888-706-1535 and speaking to a case worker
Are you eligible?
There are several ways to apply for Medicaid, Healthy Montana Kids Plus and Healthy Montana Kids programs:
- Apply online at apply.mt.gov
- Contact the Offices of Public Assistance (OPA) for questions about applications and/or eligibility at 1-888-706-1535
- Email for an application
- Download Spanish Language Application
Standard Benefits Include:
- Breast pumps
- Dental care
- Doctor, hospital, and emergency services
- Family planning
- Home health services
- Laboratory and x-ray services
- Maternity and newborn care
- Mental health and substance abuse treatment
- Prescription drugs
- Rehabilitative services and supplies
- School-based services
- Speech therapy, audiology, and hearing aids
- Transportation to appointments
- Vision care
For more detailed information regarding benefits, check the Montana Healthcare Programs Member Guide.
Passport to Health (Passport): Choose your primary care provider
Passport is the primary care case management (PCCM) program for Montana Medicaid and HMK Plus members. The Passport programs support Medicaid and HMK Plus members, as well as providers, to establish a strong doctor/patient relationship and ensure the appropriate use of services.
- You can choose your Passport provider anytime online.
- If you do not choose a Passport provider, you will be assigned one.
- If you need help choosing your Passport provider or have questions regarding Passport, call the Medicaid/HMK Plus Member Help Line at 1-800-362-8312, M-F, 8am-5pm.
- Remember, you will need a referral (approval) from your Passport provider before you can see most other healthcare providers.
- For more Passport information, see the Passport Section of the Member Guide.
Member Rights and Responsibilities
Missed or Canceled Appointments
When members do not show up for a scheduled appointment, it creates an unused appointment slot that could have been used for another member. It is very important to keep appointments and call the provider in advance if you cannot make it to a scheduled appointment. Medicaid providers cannot bill a member for no-show/missed appointments. However, a provider may discharge a member from their practice after so many no-show/missed appointments. The provider must have the same policy for Medicaid members as non-Medicaid members, and must notify Medicaid members that the policy exists.
For a full list of member rights and responsibilities, see the Member Rights and Responsibilities Section of the Member Guide.
Need help finding your local Office of Public Assistance, Enrolled Medicaid Provider, or Passport Provider? Call Montana Healthcare Programs, Member Help Line 1-800-362-8312, M-F, 8am-5pm, for assistance.
Find a Montana Medicaid Provider.
Find a Montana Medicaid or HMK Plus Dental Provider.
Report a change for your case or apply for healthcare coverage.
View details about your case.
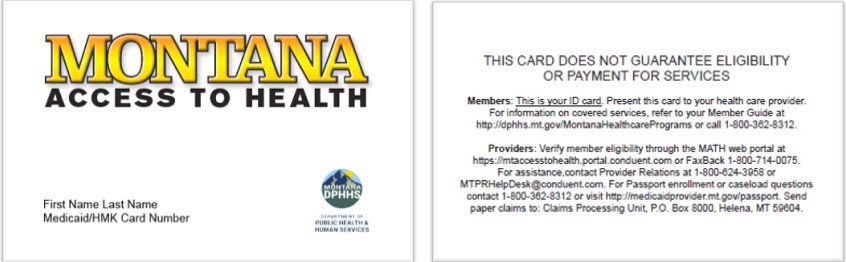
If you lost your Medicaid/HMK Plus Card, call 1-888-706-1535 for a replacement.
Member Education - Newsletters and Guides
Do you still have questions?
Here is a copy of the Montana Healthcare Programs Member Guide. Be sure to check the announcements section above for information on changes to your benefits.
Public Assistance Help Line
Eligibility and reporting changes to your case
1-888-706-1535
Medicaid/HMK Plus, Member Help Line
Medical Benefits, copayments, and Passport to Health questions
1-800-362-8312
Medicaid Transportation Services
Contact the Medicaid Transportation Center
1-800-292-7114

