Zoonotic Diseases
Zoonotic diseases are infections that are spread between animals and humans. Animals are an important part of the lives of Montanans- whether it’s a beloved family pet, livestock, or wildlife, it’s important to stay safe when handling animals. Learn more about zoonotic diseases and how to keep yourself and your family safe below.
Zoonotic diseases spread by 5 primary routes: direct contact, indirect contact, foodborne, vector-borne, and waterborne.
- Direct Contact: Coming into contact with the saliva, blood, urine, mucous, feces, or other body fluids of an infected animal. Examples include petting or touching animals, bites or scratches, and field dressings or skinning carcasses.
- Indirect Contact: Coming into contact with areas where animals live and roam, or objects or surfaces that have been contaminated with germs. Examples include aquarium tank water, pet habitats, chicken coops, barns, plants, soil, pet food and water dishes, and pet toys.
- Foodborne: Each year, 1 in 6 Americans get sick from eating contaminated food. Eating or drinking something unsafe, like unpasteurized (raw) milk, undercooked meat or eggs, or raw fruits and vegetables that are contaminated with feces from an infected animal may result in zoonotic disease.
- Vector-Borne: Being bitten by a tick or an insect like a mosquito or a flea.
- Waterborne: Drinking or coming into contact with water that has been contaminated with feces from an infected animal.
Examples of zoonotic diseases include rabies, hantavirus, Q fever, brucellosis, chronic wasting disease, psittacosis, melioidosis, Colorado tick fever, Lyme disease, malaria, tularemia, highly pathogenic avian influenza, parasitic conditions such as echinococcosis, and a few foodborne illnesses.
- Always wash your hands with soap and water after interacting with animals, animal body fluids, things animals have touched, or places where animals are housed.
- Avoid touching your eyes, nose, and mouth after interacting with animals.
- Consume pasteurized milk and dairy products. When travelling to other countries, avoid dairy and milk products if you’re not certain that they’re pasteurized.
- Follow the 4 steps to food safety: clean, separate, cook, and chill.
- Don’t eat or drink around animals.
- Keep livestock and live poultry outside of the home.
- Supervise small children and infants when they’re around animals.
- Hunters and trappers should wear gloves when field dressing or skinning wildlife and cook game meat to an internal temperature of 165 F.
Zoonotic Diseases in Montana
MTDPHHS works closely with the Department of Livestock to monitor trends in zoonotic diseases in Montana. This interagency collaboration allows both departments to identify and mitigate cases of zoonotic diseases in both animal and human populations, supporting a healthier community in Montana. Learn more about zoonotic diseases that MTDPHHS actively monitors below!
Q fever is a zoonotic disease caused by the bacteria Coxiella burnetii. The bacteria can aerosolize easily and result in infection if someone inhales it. This typically happens when someone is assisting with animal birthing or if dust is disturbed and aerosolized. Another common place of exposure occurs in abattoirs. Q fever can also be transmitted if the bacteria come into contact with a mucous membrane (mouth, nose, eyes) or an open wound. If an animal is infected with Q fever and is producing milk for raw milk consumption, it’s possible that the milk is contaminated with bacteria and may result in infection.
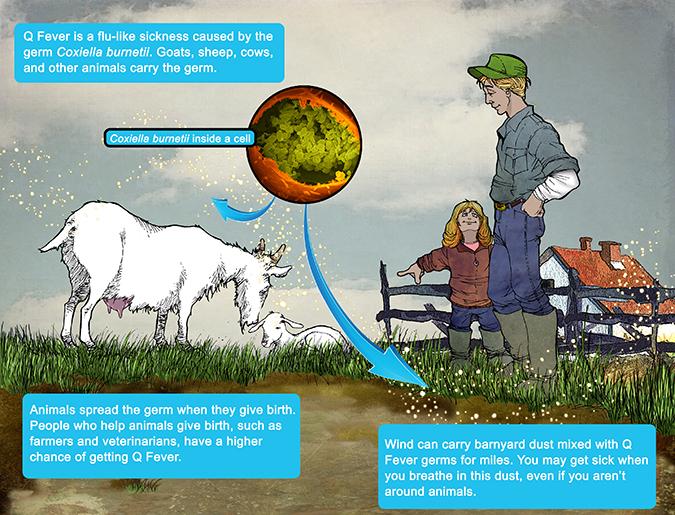
Symptoms of Q fever include fever, chills, fatigue, headaches, muscle aches, nausea, vomiting, diarrhea, chest pain, stomach pain, and weight loss. Women who are infected during pregnancy may be at risk for miscarriage, stillbirth, pre-term delivery, or low infant birth weight. Q fever can progress to a serious, and sometimes life threatening, condition that causes heart swelling (endocarditis) if left untreated. It is important to seek medical care immediately if you suspect that you have symptoms of Q fever following a possible exposure.
Montana has reported 44 cases of Q fever since 2008 (figure 1). The average age of individuals infected with Q fever in Montana is 50 years-old (range 11-79 years-old, median age of 50 years).
Figure 1. Reported Q Fever Cases in Montana by County of Residence, 2008-2023 (n=44)
In 2011, a multi-state outbreak of Q fever was identified that was associated with a goat farm in Washington state. Fifteen cases of Q fever in Montana were linked to this outbreak (figure 2). Cases identified from this outbreak comprise 34% of the total number of cases reported in Montana between 2008 and 2023. Montana has reported one death due to Q fever since 2008.
Figure 2. Q Fever Cases by Disease Outcome, Montana, 2008-2023
Brucellosis is a zoonotic disease that may be caused by multiple species of bacteria in the Brucella genus. People can get the disease when they come into contact with contaminated animal products, such as birthing fluids, abortion products, or vaginal discharge from an infected animal. When sheep, goats, cows, or camels are infected, their milk can become infected with the bacteria that cause brucellosis. If the milk from these animals is not pasteurized (raw), the infection may be transmitted to the people who consume contaminated raw milk products. Due to the presence of brucellosis in wildlife in the Greater Yellowstone Area, Montana has a Designated Surveillance Area (DSA) to monitor cattle and domestic bison for spillover infections from wildlife. The DSA includes parts of the following counties: Park, Gallatin, Madison, and Beaverhead. For more information on management of brucellosis in wildlife and livestock, please visit Montana Fish Wildlife and Parks and the Montana Department of Livestock.
Human cases of brucellosis are low incidence in Montana, meaning that there are very few cases that are reported annually. Montana has not officially reported a case of human brucellosis since 2017*, but there have been two human cases of provider-diagnosed Brucellosis reported in Montana in 2023. Both cases reported recent travel out of the country and consumption of raw milk products. These cases are not being officially counted as Montana cases due to their residency classifications and the type of testing performed for diagnosis.
*Note: MTDPHHS follows case definitions established by the Council for State and Territorial Epidemiologists (CSTE) when determining if an individual meets the requirements to be counted as a case of a communicable disease. A provider may still diagnose a patient with a case of a communicable disease even if MTDPHHS does not classify nor count them as a case.
MTDPHHS works closely with the Department of Livestock to monitor and investigate individuals who may have been exposed to Brucella canis. Over the past year, canine disease prevalence has increased and there is a broader geographic distribution of dogs testing positive for B. canis throughout Montana.
B. canis can infect humans, although it is very rare. The most common way humans become infected is through direct contact with birthing fluids, canine abortion products, or vaginal discharge from an infected dog since large amounts of B. canis bacteria may be found in these substances. Laboratory personnel, veterinarians, breeders, and animal caretakers are the groups with the greatest B. canis exposure risk due to the nature of their occupations. The risk of contracting brucellosis from B. canis in a household setting from simply touching a dog bowl or toy is incredibly low, especially if you practice good hand hygiene afterwards. Infants and children may have a slightly higher risk due to having an immature immune system and being unaware of proper hygiene practices, such as good hand washing and avoiding mouthing. Immunocompromised individuals may be at greater risk of contracting brucellosis.
The following recommendations should be followed regardless of if a dog is suspected of being infected or sick:
- Wash your hands with soap and water for at least 20 seconds after interacting with an animal. If soap and water are not readily available, use an alcohol-based hand sanitizer. Dry your hands with a clean disposable towel or napkin.
- Animal caretakers, especially those working with breeding dogs, newborn puppies, or aborted fetuses, should always wear latex or rubber gloves when handling bodily fluids (e.g., birthing or reproductive secretions, urine, saliva, and tissues) from an animal. Consider using eye protection and covering any scratched skin or open wounds to prevent splash exposures. Do not administer mouth-to-mouth resuscitation on stillborn pups.
- When disinfecting kennel areas and runs, face masks and eye protection should be worn to prevent any material from entering the mouth, nose, or eyes.
In Montana, hantavirus is primarily spread by deer mice but can also be spread by the white-footed mouse in eastern Montana. Someone exposed to hantavirus might develop hantavirus infection which could progress to a severe disease called hantavirus pulmonary syndrome (HPS). Learn more about hantavirus infection on our Hantavirus webpage.
Raising backyard birds has become an increasingly popular activity in Montana, and can provide many fun and educational benefits. However, there are some associated health risks that should be considered while interacting with live poultry.
Live poultry can carry germs such as Salmonella and Campylobacter, even if they appear clean and healthy. These types of germs can cause humans to get sick with symptoms including diarrhea, stomach pain, fever, and sometimes vomiting. In 2023, 72 salmonellosis and campylobacteriosis cases in Montana reported contact with live poultry before their illness started, 11 of whom were hospitalized due to their infection.
Follow these prevention steps below to keep you and your family healthy while interacting with backyard birds:
- Always wash your hands with soap and water right after handling eggs, backyard poultry, or anything in their environment.
- Avoid touching dead, injured, or sick backyard poultry.
- If you must handle a wild bird or sick or dead poultry, take protective measures. Do not handle the animal with bare skin. Wear gloves and wash your hands thoroughly with soap and water after contact. Respiratory protection (such as a facemask) and eye protection (such as goggles) are also highly recommended.
- Supervise children around poultry, and make sure they wash their hands after contact.
- Avoid eating or drinking in areas where poultry live or roam.
- Avoid kissing or snuggling your birds.
- Keep chicks and ducks outside of the home.
- Set aside a pair of shoes to wear while taking care of backyard birds, and keep those shoes outside of the house.
Hunters in Montana
Hunting is an integral part of the lives of many Montanans, and there are great reasons why: we have some of the longest hunting seasons in the West, plenty of healthy and diverse herds of game, and access to millions of acres of public and private land. MTDPHHS wants you to enjoy the hunting season while staying safe and healthy. Follow the steps below while hunting to keep you and your loved ones safe.
- Before leaving for your hunt, familiarize yourself with animal-specific hunting regulations published by Montana Fish, Wildlife, and Parks as they contain valuable information regarding safe carcass disposal.
- Do not eat, drink, or smoke while cleaning wild fowl or game.
- If possible, protect your hands with gloves (heavy rubber, latex, or nitrile) when field dressing wild game or fowl. Always wash your hands with soap and water after handling wild game or fowl, even if you wore gloves. If you do not have access to soap and water, make sure you have an alcohol-based hand sanitizer readily available.
- Wash all tools, equipment, and working surfaces thoroughly with soap and water, followed by disinfection immediately after handling any wild game or fowl. Adding a minimum of 1 tablespoon of bleach to 1 gallon of water is usually adequate for use as a cleaning/disinfecting solution.
- If any viscera (internal organs) have an abnormal appearance, smell, or discharge, or if pockets of blood are seen in muscle unassociated with the bullet/shot/arrow wound, the flesh should be considered unfit for eating.
- Avoid eating raw or undercooked meat.
- Any uncooked game should be promptly frozen, refrigerated, or disposed of properly.
- Report any signs of sick wildlife or wild bird die-off to Montana Fish, Wildlife, and Parks.
- Hunters in Montana can have their deer, elk, or moose tested for chronic wasting disease with the help of Montana Fish, Wildlife & Parks. FWP is paying for the testing of samples. CWD sampling is voluntary. In Priority Surveillance Areas, sampling is strongly encouraged to help FWP gather additional data to inform management.
- Hunters can either take the samples themselves, fill out the online hunter submission form and mail them to our Wildlife Health Lab in Bozeman, or they can bring the animal (or head) to an FWP regional office or CWD Sampling Station. Hunters who visit a regional office should be prepared to experience wait times during busy hours. Check with your regional office for optimal times, but in general regional offices will be able to take samples during normal business hours. Outside of the general deer and elk season, please call your regional office ahead of time to schedule a time to have your animal sampled. For more information, visit: Montana Fish, Wildlife, and Parks 'Get Your Animal Sampled' page.
Department of Livestock- Canine Brucellosis
Q&A for Dog Owners: Canine Brucellosis- PDF
Species-Specific Guidance for Hunters in Montana
Rabies in Montana- Department of Public Health
Rabies in Montana- Department of Livestock
CDC: Healthy Pets, Healthy People