COVID-19, Influenza, and RSV

Current Activity
The Montana Communicable Disease Epidemiology Section maintains a dashboard that summarizes current data for COVID-19, influenza, and RSV activity in Montana. This dashboard is updated weekly to provide Montanans with the most current data for these conditions.
View the Pan-Respiratory Dashboard for COVID-19, influenza, and RSV.
About Viral Respiratory Illnesses
- Respiratory viruses are responsible for thousands of illnesses every year in Montana. In addition to the virus that causes COVID-19, the influenza virus and respiratory syncytial virus (RSV) are common viruses that circulate annually. Parvovirus B19 (Fifth Disease), adenovirus, rhinovirus, and parainfluenza are also common viruses that circulate annually.
- COVID-19, influenza (flu), and RSV are common circulating respiratory conditions in Montana. They are caused by different viruses and are different diseases: SARS-CoV-2 (COVID-19), influenza viruses (flu), and respiratory syncytial virus (RSV).
- These viruses spread between people when someone who is sick coughs, sneezes, or does other things to cause droplets containing the virus to be expelled.
- These viruses spread year-round, but activity tends to peak in the fall, winter, and spring months (e.g., October-May).
| Common Symptoms | COVID-19 | Flu | RSV | Cold |
|---|---|---|---|---|
| Fever and/or chills | Yes | Yes | Yes | No |
| Headache | Yes | Yes | No | No |
| Muscle pain or body aches | Yes | Yes | No | No |
| Feeling tired or weak | Yes | Yes | No | No |
| Sore throat | Yes | Yes | No | Yes |
| Runny or stuffy nose | Yes | Yes | Yes | Yes |
| Sneezing | No | No | No | Yes |
| Cough | Yes | Yes | Yes | Yes |
| Shortness of breath | Yes | Yes | Yes | No |
| Vomiting or diarrhea | Yes | Yes | No | No |
| Change in or loss of taste or smell | Yes | No | No | No |
- Symptoms of COVID-19, flu, RSV, and other respiratory illnesses are similar and may include a fever, cough, sore throat, runny or stuffy nose, headache, body aches, and low energy.
- If you are experiencing any of these symptoms, consult with your medical provider. Your provider may recommend that you get tested to confirm a diagnosis.
- If you are experiencing an emergency warning sign (such as trouble breathing or chest pain), seek medical care immediately.
- Testing is an important tool to help protect yourself and others from COVID-19, influenza, and RSV infections.
- Testing for respiratory viruses can help you decide what to do next, like seeking treatment to reduce your risk of severe illness or taking steps to lower your chances of spreading viruses to others.
- COVID-19 tests are available over the counter and from community testing sites.
- A healthcare provider can help advise you on getting tested for flu, COVID-19, RSV, or other respiratory viruses.
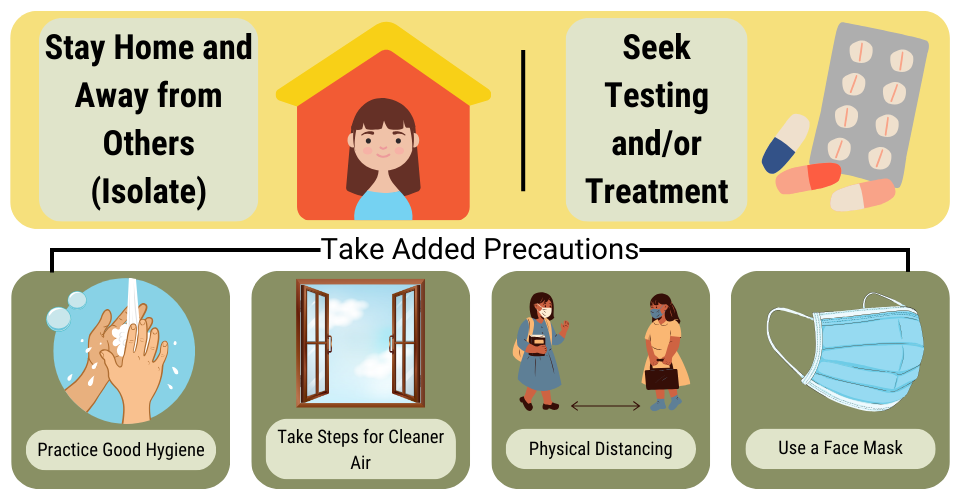
Stay Home and Away from Others (Isolate)
- You may return to your normal daily tasks when you are experiencing an improvement in symptoms and have been fever-free for at least 24 hours without the use of a fever-reducing medication (e.g., Tylenol).
Seek Health Care for Testing and/or Treatment
- Treatments for COVID-19 and the flu can help lessen symptoms and shorten the time that you are sick. They may also reduce the risk of complications, including those that can result in hospitalization. For individuals at risk for severe illness, early treatment can result in a milder illness.
Use Additional Precautions for 5 Days After Returning to Normal Activities
- Practice good hygiene
- Hygiene (practices that improve cleanliness) is a core prevention strategy to lower risk from respiratory viruses.
- Practice good hygiene by covering your coughs and sneezes, washing or sanitizing your hands often, and cleaning frequently touched surfaces.
- Take steps for cleaner air
- Respiratory viruses can spread in the air between people. By bringing in fresh outside air, purifying indoor air, or gathering outdoors, you can improve air quality and possibly lower your risk of contracting a respiratory virus.
- Maintain physical distance
- Infectious droplets and particles build up in the air closer to the person who is releasing them. Putting physical distance between yourself and others can help lower the risk of spreading respiratory viruses.
- Wear a mask
- Wearing a mask can help lower the risk of spreading respiratory viruses. When worn by a person who is currently sick or is beginning to feel better after being sick, masks reduce the spread of the virus to others by preventing respiratory droplets from circulating in the air.
- Immunizations are a core prevention strategy for reducing the total number of cases and overall risk of severe illness from respiratory illness.
- Immunizations work in two different ways depending on the type you receive. One way immunizations work is by showing your immune system what the virus looks like so your body can develop antibodies to fight it. The other way immunizations work is by directly giving your body antibodies. Antibodies can help prevent infection. If you do become infected, antibodies help shorten the length of your illness and can reduce your risk of severe health outcomes like hospitalization and death.
- Immunizations are especially important for individuals who are at risk of severe illness. This includes older adults, young children, people with weakened immune systems, people with disabilities, and pregnant women.
- Talk with a healthcare provider to make sure you are up to date on your immunizations.
- COVID-19
- Flu
- There are several FDA-approved antiviral drugs recommended by the CDC to treat flu this season for people who are very sick with flu illness, and those with flu or suspected flu and who are at higher risk of serious flu complications (e.g., people with asthma, diabetes, or heart disease).
- Oseltamivir phosphate (available as a generic version or under the trade name Tamiflu)
- Zanamivir (Relenza)
- Peramivir (Rapivab)
- Baloxavir marboxil (Xofluza)
- Flu treatments are most effective when started within 2 days of getting sick. However, starting them later can still be beneficial.
- There are several FDA-approved antiviral drugs recommended by the CDC to treat flu this season for people who are very sick with flu illness, and those with flu or suspected flu and who are at higher risk of serious flu complications (e.g., people with asthma, diabetes, or heart disease).
Additional Resources
Schools can help prevent infections caused by common childhood respiratory or stomach viruses by using and encouraging everyday actions.
- Take steps for cleaner air
- Move group activities outside when possible, including lunch, certain classes, and recess/social periods.
- Cleaning, sanitizing, and disinfecting
- Schools should follow procedures for routine cleaning, sanitizing, and disinfecting.
- Rarely, a school may need specialized or enhanced cleaning and disinfection for a particular infectious disease (e.g., norovirus). Schools should consult with their local or tribal health department to determine what cleaning and disinfection is needed in these instances.
- When and How to Clean and Disinfect a Facility
- Hand washing
- Teaching and reinforcing proper handwashing and hand hygiene can lower the risk of spreading diseases.
- Schools can set routines and scheduled opportunities for handwashing throughout the day (e.g., coming inside after recess, before lunch, etc.).
- Schools should provide adequate handwashing supplies (e.g., soap, water, and paper towels). If soap and water are not available, an alcohol-based hand sanitizer with at least 60% alcohol should be provided.
- Remember to store hand sanitizers up, away, and out of sight of younger children!
- Respiratory etiquette
- Schools should reinforce the covering of the mouth and nose with a disposable tissue when someone needs to cough or sneeze.
- If tissues aren't available, students and staff should cover their mouth and nose with their elbow, not their hands.
- Handwashing should be followed immediately after blowing the nose, coughing, or sneezing.
- Vaccinations
- Vaccinations and immunizations are safe and effective tools that provide protection against COVID-19, influenza, and RSV.
- All states, including Montana, have vaccination requirements for children attending schools and daycares.
- Schools should provide information about recommended vaccines to staff, students, and families.
- Schools can also consider making vaccinations available on-site by hosting school-located vaccination clinics.
Know that the emergency warning signs of respiratory virus complications can be different in children. Seek immediate medical care for any of the following:
-
Fast breathing or trouble breathing
-
Bluish lips or face
-
Ribs that pull in with each breath
-
Chest pain
-
Severe muscle pain (for example, child refuses to walk)
-
Dehydration (no urine for 8 hours, dry mouth, no tears when crying)
-
Lack of alertness or interacting when awake
-
Seizures
-
Fever above 104 degrees Fahrenheit that is not controlled by fever-reducing medicine
-
In children younger than 12 weeks, any fever
-
Fever or cough that improves but then returns or worsens