West Nile Virus
WNV has been detected in Montana for the 2025 summer season. This increases risk of WNV exposure in humans and horses across the state – remember to prevent mosquito bites!
Active WNV season is currently underway in Montana. Across 37 counties in the state, mosquitoes have been trapped for WNV testing. When a group of mosquitoes are collected in one trap, they are referred to as a mosquito “pool”. During the majority of WNV seasons in Montana, WNV is detected in mosquito pools before the first seasonal cases are identified in humans or horses. Mosquito surveillance in Montana is an early warning system for WNV activity.
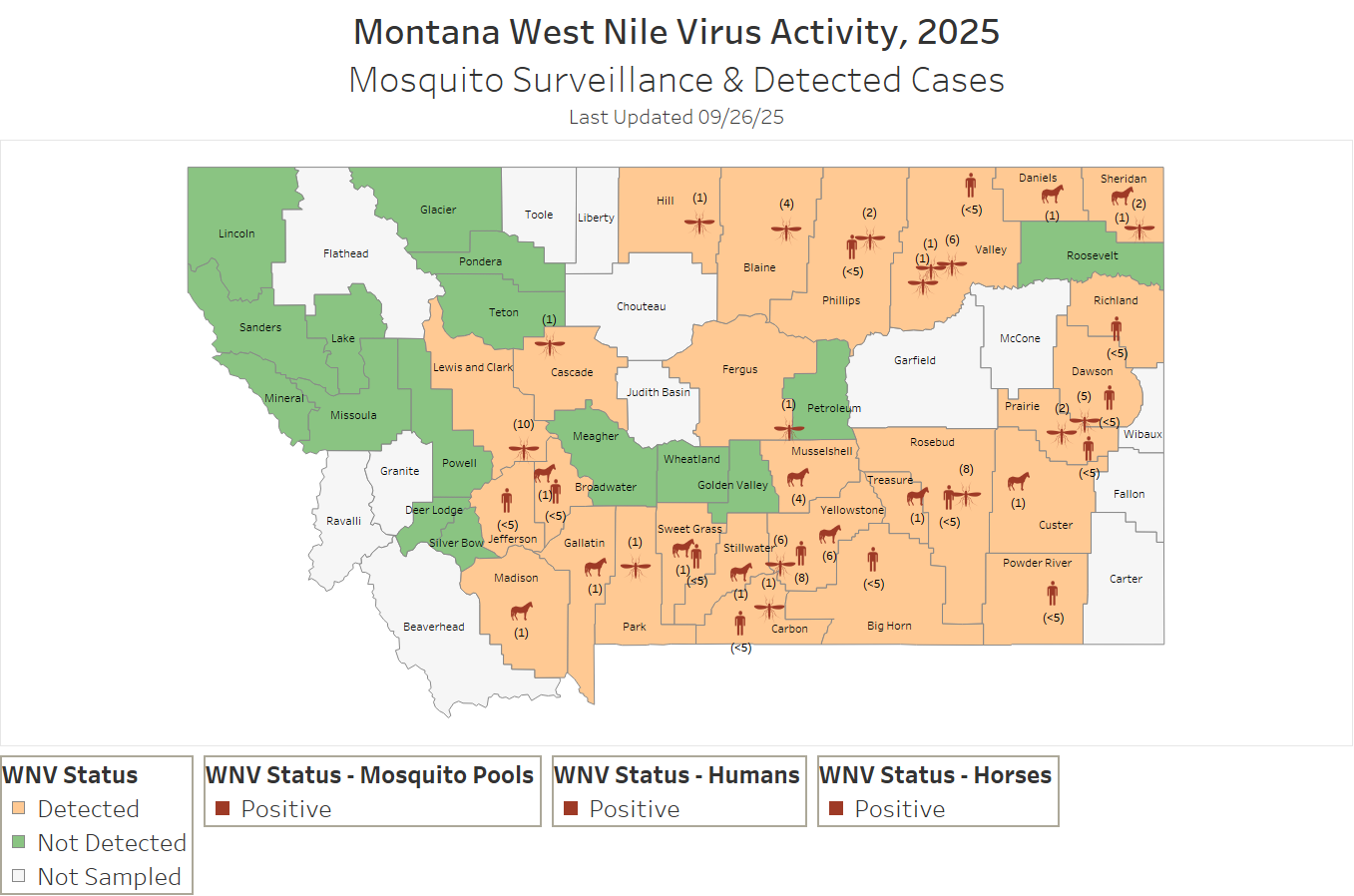
The map above displays WNV surveillance and activity for the 2025 season in Montana. It is updated on a weekly basis or as new data is collected. Orange counties and icons show where WNV detections have occurred in Montana for the 2025 season and green counties show areas where mosquito pools have been collected and tested negative for WNV. Grey counties are areas where mosquito surveillance has not occurred yet this season. Red icons show positive cases of humans, horses, and mosquito pools. Mosquito pools are shown in the approximate region of collection. Human and horse icons are placed randomly within the county of residence.
More Information about WNV
WNV is a virus that can be transmitted to humans following the bite of an infected mosquito. First introduced to the US in 1999 and Montana in 2002, WNV is a flavivirus closely related to viruses such as dengue, yellow fever, and Zika. The primary carriers of WNV are Culex species mosquitoes, also called house mosquitoes. Currently, WNV is the only mosquito-borne illness considered established in Montana.
There are multiple forms of illness for WNV, including: asymptomatic, non-neuroinvasive, and neuroinvasive illness. Following a bite from an infected mosquito, symptoms of WNV will typically show after 2 to 6 days but may be as long as 14 days following exposure. Thankfully, current evidence shows that immunocompetent people can only be infected with WNV once. One infection results in lifelong immunity. After testing positive for WNV, it’s likely that you will continue to test positive for certain types of WNV antibody for years after your infection.
WNV is not transmitted person to person. Coughing, sweating, sneezing, or otherwise interacting with another person while sick with WNV will not spread the disease. However, WNV can be unintentionally transmitted through blood and organ donation. Blood banks currently screen donations for WNV In an effort to prevent WNV transmission through blood donation. If you have been diagnosed with WNV, you should wait 120 days before donating blood. Do not donate blood if you don’t feel well.
Many people may never know they were infected with WNV – about 4 in 5 people will not show symptoms while they’re infected. However, about 1 in 5 people develop a mild form of illness known as “West Nile fever” or “non-neuroinvasive West Nile”. With non-neuroinvasive WNV, while the symptoms tend to be minor and include fever, rash, body aches, headache, arthralgia, and myalgia, many individuals experience difficulty with long-term fatigue following infection. In some cases, non-neuroinvasive illness can lower activity levels for weeks to months, making it extremely difficult to work or play.
Approximately 1 in 150 people (less than 1%) develop neuroinvasive WNV. Neuroinvasive WNV is a very serious illness, sometimes resulting in long-term disability (e.g. paralysis, blindness), encephalitis, meningitis, and/or death. Symptoms of neuroinvasive WNV include:
- High fever
- Headache
- Neck stiffness
- Stupor
- Disorientation
- Coma
- Tremors
- Convulsions
- Muscle weakness
- Vision loss
- Numbness
- Paralysis
Symptoms may persist for several weeks or may be permanent. It is not currently known what causes different people to have such different symptoms, however age is a risk factor. Over the age of 60, the chance of developing neuroinvasive WNV increases to 1 out of 50 infected individuals. There is no targeted treatment for WNV.
If you believe you have a West Nile virus infection, contact your physician.
The best way to prevent WNV infection is to prevent getting bitten by mosquitoes. You can take steps to minimize your possibility of encountering WNV (and sometimes mosquitoes!) by remembering the 4Ds of WNV Prevention:
- DRESS: Wear shoes, socks, long pants, and a long-sleeved shirt when outdoors for long periods of time or when mosquitoes are most active. Clothing should be light colored and made of tightly woven materials to keep mosquitoes away from the skin.
- DRAIN: Reduce the amount of standing water in or near your property by draining and/or removing it. Mosquitoes may lay eggs in areas with standing water. Necessary standing water should be changed (e.g. birdbath), moved (e.g. adding a fountain to a pond), or covered (e.g. putting a mesh screen over a water barrel).
- DEET: For additional protection from mosquitoes, use an insect repellent containing DEET (N,N-diethyl-m-toluamide) or picaridin (KBR 3023). Other insect repellents such as oil of lemon eucalyptus and IR3535 are also registered by the EPA but may be less effective than products containing DEET. It is important to follow the product guidelines when using insect repellent.
- DAWN/DUSK: Whenever possible, avoid spending time outside at dawn and dusk. This is when the mosquitoes that spread WNV are most likely to bite. If you keep windows open in your home, make sure that you are using well-fitting screens without holes or tears, to prevent mosquitoes from coming inside.
WNV in Montana
Mosquitoes belonging to members of the Culex species are the most common vectors of WNV in North America. In Montana, Culex tarsalis is the most common WNV mosquito vector. Not all types of mosquitoes carry all mosquito-borne illnesses. This is why WNV is Montana’s primary mosquito-borne illness, but many others like Zika, Yellow Fever, Eastern Equine Encephalitis, Malaria, are not currently acquired in this state.
The first confirmed case of WNV in MT was detected in a horse in July 2002, followed shortly by the first human case in August 2002. As a novel illness to many Montanans at the time, Montana experienced it’s worst WNV outbreak in 2003 with over 200 cases detected. Outbreaks now occur every few years, with human detections spiking again in 2007, 2013, 2018, and 2023.
Annually, the MT DPHHS contracts mosquito surveillance for WNV. This activity includes collecting mosquitoes from around the state and testing them for WNV. Once WNV is detected, MT DPHHS puts out notice. Each season, the first cases of WNV infection in humans and horses are typically reported about two weeks after the first detection of WNV in mosquito pools.
If you have recent exposure to mosquitoes and develop symptoms compatible with WNV, reach out to your provider. Your provider may consider testing for WNV. However, also alert your provider if you have traveled out of state in the last 14 days before your symptoms started, as you may have been exposed to other mosquito-borne illnesses that are more prevalent in the areas where you traveled. This will help your provider in knowing what testing to consider.
If you have not traveled outside of Montana and you test negative for active WNV infection, your provider may also consider testing for: Jamestown Canyon virus, Snowshoe Hair virus, St. Louis Encephalitis, or Western Equine Encephalitis. However, these mosquito-borne viruses have not been detected in Montana in many years – or at all.
Click on the year of interest below to learn more about WNV cases and distribution in MT.
| Year | Humans | Deaths | Horses |
|---|---|---|---|
| 2023 | 42 | 1 | 22 |
| 2022 | 0 | 0 | 2 |
| 2021 | 2 | 0 | 2 |
| 2020 | 1 | 0 | 1 |
| 2019 | 4 | 0 | 2 |
| 2018 | 51 | 1 | 50 |
| 2017 | 13 | 0 | 8 |
| 2016 | 7 | 2 | 7 |
| 2015 | 3 | 0 | 4 |
| 2014 | 5 | 0 | 3 |
WNV in Horses
WNV infection in horses can also cause severe illness or death. Horses are infected with WNV through the bite of an infected mosquito, much like humans. Reported annual cases of WNV in horses in Montana range from as few as 1 in 2020 to 50 in 2018. Horses have an annual WNV vaccine available, and vaccination is highly encouraged core vaccine and is an essential standard of care for all horses in North America. Horses vaccinated against Eastern, Western, and Venezuelan equine encephalitis are not protected against infection with WNV. Talk your veterinarian if you would like more information about WNV vaccination for horses. You can also check out the Montana Department of Livestock’s website for more information about horses and WNV, including annual trends.

