Chlamydia

Chlamydia is caused by the bacterium Chlamydia trachomatis and was the most common sexually transmitted infection (STI) in Montana and the United States. Chlamydia infections are often asymptomatic and may go unnoticed. However, a chlamydia infection can cause permanent damage to a woman's reproductive system, and can make it difficult or impossible to get pregnant later. Chlamydia can also cause a potentially fatal ectopic pregnancy (pregnancy that occurs outside the womb).
Screening is recommended at least annually, and sometimes more often, if you are a woman under the age of 25, a woman at risk of a sexually transmitted infection, or a man who has sex with men.
- How do I know if I have it?
- Am I at risk?
- Prevention
- I'm pregnant. If I have chlamydia, how can I protect my baby from getting it?
- Should I be tested for chlamydia?
- Is there a cure for clamydia?
- What happens if I have a chlamydia infection and don't get treated?
How do I know if I have it?
Chlamydia often has no symptoms, but it can cause serious health problems, even without symptoms.
Women with symptoms may notice an abnormal vaginal discharge and/or a burning sensation when peeing. Men with symptoms may notice a discharge from their penis and/or a burning sensation when peeing.
Men and women can get chlamydia in their rectum. This happens either by having receptive anal sex, or by spread from another infected site (such as the vagina). These infections are often asymptomatic. People with symptoms may notice rectal pain, discharge, or bleeding.
See your healthcare provider if you notice any of these symptoms or if your partner has an STI or symptoms of one.
Am I at risk?
Sexually active people can get chlamydia through vaginal, anal, or oral sex without a condom with a partner who has chlamydia. Women who are pregnant can give the infection to their baby during childbirth.
If you are sexually active, have an honest and open discussion with your healthcare provider. Ask them if you should get tested for chlamydia or other STIs.
Prevention
The only way to completely avoid STIs is to not have vaginal, anal, or oral sex. If you are sexually active, you can lower your chances of getting chlamydia by using condoms the right way and being in a long-term, mutually monogamous relationship with a partner who has been tested and does not have chlamydia.
I'm pregnant. If I have chlamydia, how can I protect my baby from getting it?
If you are pregnant and have chlamydia, you can give the infection to your baby during delivery. This can cause serious health problems for your baby. If you are pregnant, talk to your healthcare provider about getting the correct examination, testing, and treatment. Treating chlamydia as soon as possible will make health problems for your baby less likely.
Should I be tested for chlamydia?
If you are sexually active, have an honest and open talk with your healthcare provider. Ask them if you should get tested for chlamydia or other STIs.
If you are a sexually active gay or bisexual man, you should get tested for chlamydia every year. People living with HIV, on HIV PrEP, who have multiple partners, or have a partner with multiple partners should be tested every 3-6 months.
If you are a sexually active woman, you should get tested for chlamydia every year if you are:
- Younger than 25 years
- 25 years and older with risk factors, such as new or multiple sex partners, or a sex partner who has a sexually transmitted infection
Testing is also recommended during pregnancy if you are:
- Younger than 25 years
- Older than 25 years and have risk factors such a new or multiple sex partners, a sex partner with an STI, or practice inconsistent condom use and are not in a mutually monogamous relationship.
Is there a cure for chlamydia?
Yes, the treatment can cure chlamydia. It is important to take all the medicine your healthcare provider gives you to cure your infection. When taken properly it will stop the infection and could decrease your chances of having problems later.
You should not have sex again until you and your sex partner(s) complete treatment. If given a single dose of medicine, you should wait seven days after taking the medicine before having sex. If given a medicine to take for seven days, wait until you final all the doses before having sex.
Repeat infection with chlamydia is common. You should receive testing again about three months after your treatment, even if your sex partner(s) receives treatment. If you have had chlamydia and took medicine in the past, you can still get it again. This can happen if you have sex without a condom with a person who has chlamydia.
What happens if I have a chlamydia infection and don't get treated?
The initial damage that chlamydia causes often goes unnoticed. However, chlamydia can lead to serious health problems.
In women, untreated chlamydia can cause pelvic inflammatory disease (PID). Some of the complications of PID are:
- Formation of scar tissue that blocks fallopian tubes
- Ectopic pregnancy (pregnancy outside the womb)
- Infertility (not being able to get pregnant)
- Long-term pelvic/abdominal pain
Men rarely have health problems from chlamydia. The infection can cause a fever and pain in the tubes attached to the testicles. This can, in rare cases, lead to infertility.
Untreated chlamydia may also increase your chances of getting or giving HIV.
Screening
Please see CDC STI Treatment Guidelines.
In women:
- Sexually active women under 25 years of age.
- Sexually active women 25 years of age and older if at increased risk.
- Retest approximately 3 months after treatment.
- Rectal chlamydial testing can be considered in females based on reported sexual behaviors and exposure through shared clinical decision making between the patient and the provider.
In pregnancy:
- All pregnant women under 25 years of age.
- Pregnant women 25 and older if at increased risk
- Retest during the 3rd trimester for women under 25 years of age or at risk
- Pregnant women with chlamydial infection should have a test of cure 4 weeks after treatment and be retested within 3 months.
Men who have sex with women:
- There is insufficient evidence for screening among heterosexual men who are at low risk of infection, however, screening young men can be considered in high prevalence clinical settings (adolescent clinics, correctional facilities, STI/Sexual Health Clinic)
Men who have sex with men:
- At least annually for sexually active MSM at sites of contract (urethra, rectum) regardless of condom use
- Every 3 to 6 months if at increased risk (i.e. MSM on PrEP, with HIV infection, or if they or their sex partner have multiple partners
Transgender and gender diverse persons:
- Screening recommendations should be adapted based on anatomy (i.e. annual, routine screening for chlamydia in cisgender women < 25 years old should be extended to all transgender men and gender diverse people with a cervix. IF over 25 years old, person with a cervix should be screened if at increased risk.
- Consider screening at the rectal site based on reported sexual behaviors and exposure
Persons with HIV:
- For sexually active individuals, screen at first HIV evaluation, and at least annually thereafter.
- More frequent screening might be appropriate depending on individual risk behaviors and local epidemiology.
Treatment
See CDC STI Treatment Guidelines
Recommended Regimens for Chlamydial Infection Among Adolescents and Adults
Doxycycline 100 mg orgally 2 times/day for 7 days
Alternative Regimens
Azithromycin 1 g orally in a single dose
OR
Levofloxacin 500 mg orally once daily for 7 days
Management Considerations
To minimize disease transmission to sex partners, person treated for chlamydia should be instructed to abstain from sexual intercourse for 7 days after single dose therapy or until completion of a 7-day regimen and resolution of symptoms, if present.
To minimize risk for reinfection, patients also should be instructed to abstain from sexual intercourse until all of their sex partners have been treated.
Persons who receive a diagnosis of chlamydia should be tested for HIV, gonorrhea, and syphilis.
MSM who are HIV negative with rectal chlamdia diagnosis should be offered HIV PrEP.
Test of cure (repeat testing 4 weeks after completing therapy) is not advised for nonpregnant persons treated with the recommended or alternative regimens, unless therapeutic adherence is in question, symptoms persist, or reinfection is suspected. Men and women who have been treated for chlamydia should be retested approximately 3 months after treatment, regardless of whether they believe their sex partners were treated; scheduling the follow-up visit at the time of treatment is encouraged. If retesting at 3 months is not possible, clinicians should retest whenever persons next seek medical care.
Doxy-PEP should be considered for future post-exposure prophylaxis.
Chlamydia in Pregnancy
Recommended Regimens for Chlamydial Infection in Pregnancy
Azithromycin 1 g orally in a single dose.
Alternative Regimens
Amoxicillin 500 mg orally 3 times/day for 7 days.
Clinical experience and published studies indicate that azithromycin is safe and effective during pregnancy. Doxycycline is contraindicated during the second and third trimesters of pregnancy.
Test of cure (i.e., repeat testing after completion of therapy) to document chlamydial eradication, preferably by NAAT, at approximately 4 weeks after therapy completion during pregnancy is recommended because severe sequelae can occur among mothers and neonates if the infection persists. In addition, all pregnant women who have chlamydial infection diagnosed should be retested 3 months after treatment.
Expedited Partner Therapy (EPT)
Expedited Partner Therapy (EPT) is a harm reduction strategy. It is the clinical practice of treating the sex partners of people with diagnosed chlamydia or gonorrhea, who are unable to unlikely to seek timely treatment, by providing medications or prescriptions to the patient to provide to the partner. EPT must be an oral regimen.
For more information, contact Montana STD Program stimidis@mt.gov
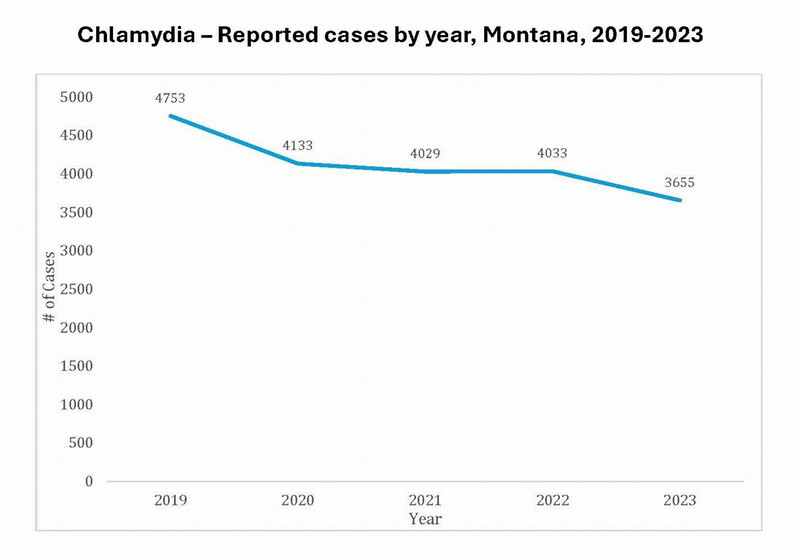
Montana Epidemiology
In 2023, there were 3,655 chlamydia cases reported in Montana.