Suicide Prevention in the Emergency Department
Introduction
Individuals in a suicide crisis regularly seek help at hospital emergency departments (ED). Additionally, EDs treat individuals with other risk factors for suicide, including substance use disorders, mental health conditions, and chronic pain.1
- The risk for suicide death or attempt is highest within 30 days of discharge from an ED or inpatient psychiatric unit.2
- Up to 70% of individuals who leave the ED after a suicide attempt do not attend their first outpatient appointment.2
- Approximately 37% of individuals without a mental health or chemical dependency diagnosis who died by suicide make an ED visit within a year of their death.3
This puts EDs in an important position to intervene and potentially save lives from death by suicide. Research has shown that there are a number of tools and interventions that have shown to reduce suicidal behavior in EDs. One study of over 1,300 ED patients with recent suicide attempts or ideation found that an intervention that incorporates screenings, assessment, discharge resources, and post-discharge follow-up resulted in a 5% decrease in the proportion of patients subsequently attempting suicide, and a 30% decrease in the total number of suicide attempts over a year follow-up period compared to usual care.4
Suicide Statistics Related to Emergency Department in Montana
According to the 2019 Montana Department of Public Health and Human Services Suicide Prevention Strategic Plan, there are more than 1,400 emergency department visits annually for intentional self-harm in Montana with women about twice as likely as men to be admitted to the emergency room with a suicide attempt.5 Additionally, the number of emergency department visits for intentional self-harm increased 40% from 2012- 2014 to 2016-2017, and the overall suicide rate in Montana rose 38% from 1999 to 2016.6 Suicide rates in Montana (25.9 per 100,000) are already almost double the national suicide rate (13.5 per 100,000).7 The State of Montana has created a strategic plan to address suicide prevention across the state, and here we provide additional resources and guidance to achieve the goals within this plan.
Emergency Departments need a program that is designed to fit an ED’s workflow and culture, while the stresses of the ED have the potential to be barriers (i.e. time pressures, boarding patients to various beds and floors, predicting imminence or severity of self-harm).
Addressing Patients at Risk for Suicide in the Emergency Department
- Brief patient education and initial safety precautions
- Conduct universal or selective.
- Provide at-risk patients with a full assessment by a mental health professional trained in effective suicide care.
- Provide brief interventions while patients are still in the ED (e.g., safety planning, lethal means counseling).
- Ensure careful discharge planning and safe transitions of care to outpatient services.
1. Brief Patient Education and Initial Safety Precautions
The Emergency Department is often an environment where levels of physical and emotional pain are higher than other health settings. Providing care that is empathetic and patient-centered should be a priority. Initial conversation with patients who enter the ED with suicidal ideation can include:
- Explaining what to expect during the ED visits and making sure basic comforts are met,
- Using a sympathetic but direct approach to enhance communication,
- Ask specific questions about the nature of suicidal thoughts, behaviors, or plans.
If a patient enters the ED because of suicidal thoughts or behaviors, it is important to keep the patient in the ED until an evaluation is complete. The patient should also be placed in a safe environment that is free of dangerous objects. The ED is a unique environment that is often associated with “crisis,” and EDs should create a written policy to clarify pathways and support provider actions for patients experiencing a suicide crisis when entering the ED.8
2. Screening
Approximately 8% of adult emergency department patients have had recent suicidal ideation or behaviors, but most individuals do not disclose this information unless they are directly asked.9 This demonstrates the importance of increased targeted or universal screening for suicide risk in the ED. When screening for suicide risk in EDs, providers should take into account a patient’s personal history, current mental state, home environment, and their specific suicidal thoughts and behaviors.
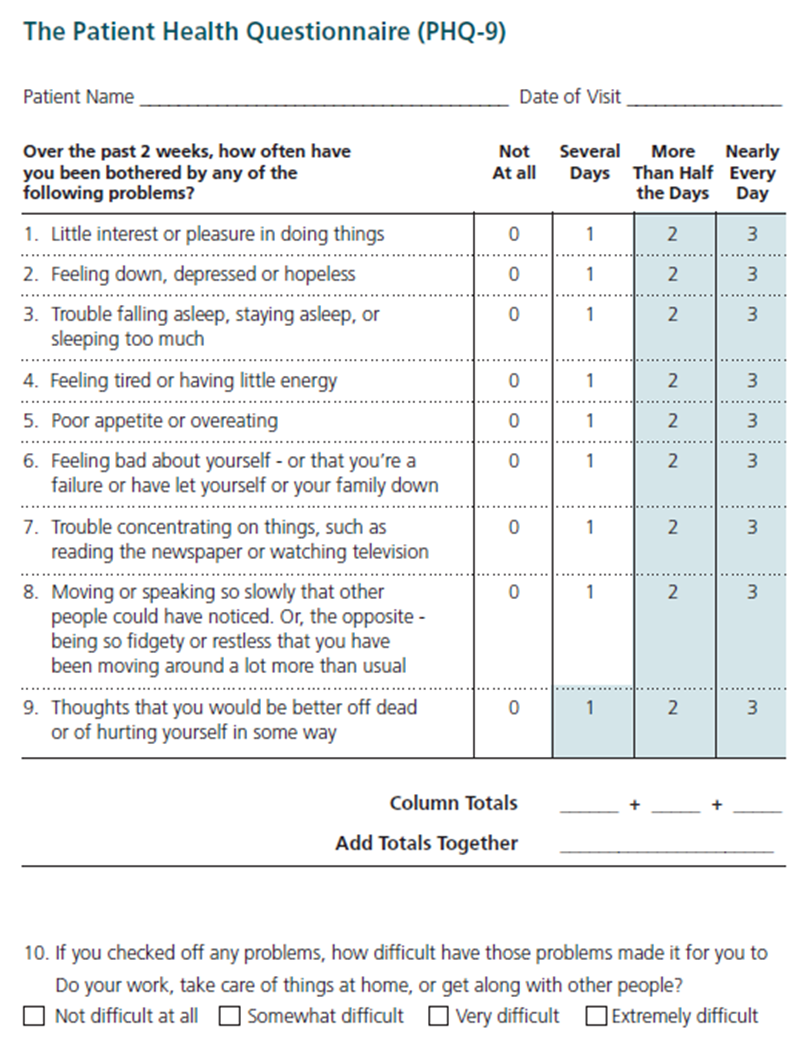
Primary Screening: Primary screening is completed with a patient to determine whether suicide risk is present or absent. Primary screening tools could include the PHQ-9 (assesses depression with specific question addressing suicidal ideation).
Patient Health Questionnaire-9 (PHQ-9): The PHQ-9 is a self-administered (but can be clinician-administered) screening tool for depression that has a specific question (Question #9) regarding suicide. The PHQ-9 is scored from 0 (not at all) to 3 (nearly every day). The PHQ-9 is shorter than other scales, can be administered in person, by telephone, or self-administered, facilitates diagnosis, provides assessment of symptom severity, is validated in a variety of populations, and can be used in adolescents as young as 12 years old.7 Question #9 specifically asks whether respondents have “thoughts that you would be better off dead or of hurting yourself in some way.” Regardless of the total score, a positive response to question #9 warrants further risk assessment.
| Severity Levels | PHQ-9 score |
|---|---|
| Normal | 0 - 4 |
| Mild | 5 - 9 |
| Moderate | 10 - 14 |
| Moderate to severe | 15 - 19 |
| Severe | 20 - 27 |
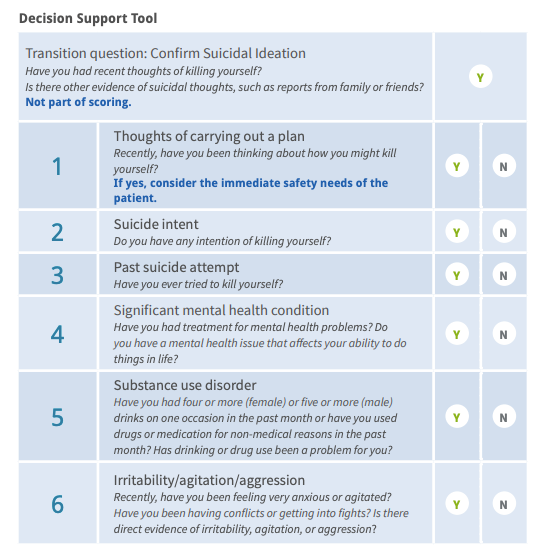
Secondary Screening: After primary screening is complete, the provider has a decision to make: does the patient need further assessment or does the information collected determine if discharge is appropriate for lower risk patients?
Lower risk patients (i.e. no suicidal intent, no previous suicide attempt, no history of mental illness or substance abuse, and no exacerbated agitation or irritability) may not need specialty care and can be managed by the ED provider.9 A 6-question Decision Support Tool is available through the Suicide Prevention Resource Center to guide providers in caring for these lower-risk patients.
3. Assessment
After preliminary screening has been completed, there may be a need for more comprehensive assessment to determine the patient’s risk and protective factors, imminent risk for suicide, and inform their treatment plan.
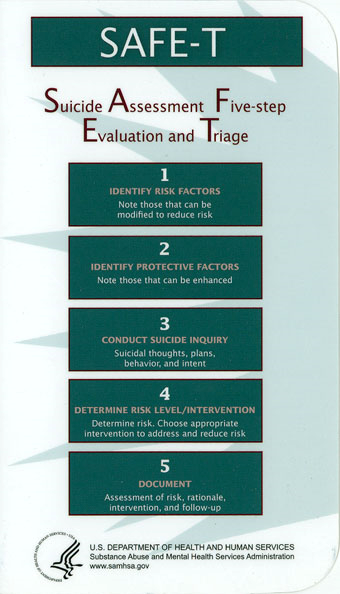
Suicide Assessment Five-Step Evaluation and Triage (SAFE-T): Typically found in the form of the SAFE-T Protocol Card, SAFE-T is a 5-step suicide assessment protocol used to address a patient’s level of suicide risk and suggest appropriate interventions. A detailed guide for the 5 steps below, with specific language and scripts, can be found here: SAFE-T Quick Guide for Clinicians
4. Interventions (Lethal Means Counseling, Safety Planning)
There are number of brief interventions that can be performed by an ED provider or specialist for patients who will be discharged from the hospital.
Lethal Means Restriction: Anyone who is identified with any level of suicide risk, from mild to severe, should be asked about access to lethal means. Removing access to lethal means for individuals at risk for suicide should be a top priority, as research shows that over 50% of suicides are completed using a firearms.11 In Montana, firearms were used in 63% of suicides in 2016.12 Providers and patients should discuss and monitor other lethal means as well, such as access to materials for hanging/suffocation (belts, ropes, or other items) or large quantities of high-risk medications.
Counseling on Access to Lethal Means (CALM): CALM is a workshop that helps providers identify patients who would benefit from lethal means counseling strategies, ask about access to lethal means, and work with patients and their family to reduce access.13 More information and guidance about which patients need counseling on access to lethal means
- For Clinicians: Sample language and steps, goals, and things to consider when talking with patients about reducing access to lethal means.
- What Clients and Families Need to Know
- Basics of Firearms
- Firearms Laws Relevant to Lethal Means Counseling
Suicide Safety Planning: Much like action plans for physical illnesses, creating a Suicide Safety Plan can be useful for patients to refer to during moments of distress. Suicide Safety Planning is evidence-based and can help patients manage suicidal thoughts and reduce emergency rooms visits. Safety Plans are created by the patient in conjunction with a provider. Safety Plans include identification of triggers and warning signs, specific activities that can steer the patient from suicidal thoughts, contacts to be used during times of distress (community, professional, and emergency), etc.
- Training for staff on how to create a safety plan is available: http://suicidesafetyplan.com/Training.html. The template for the Stanley Brown safety plan can be found here: http://suicidesafetyplan.com/Page_8.html
- Suicide Safety Planning Quick Guide
- NowMattersNow Comprehensive Safety Plan Guide
- Safety Plan pdf
- My3 is a mobile application that helps users define a network and create a plan to stay safe.
5. Careful Discharge Planning and Referral
Many patients with identified suicide risk or suicidal behaviors will be discharged from the hospital to return to the community. These patients may be considered lower risk in terms of suicide, but they may still maintain a high short-term risk for suicide. It is crucial for EDs to improve and fortify relationships between hospitals and rapidly accessible outpatient mental health resources. ED staff can also provide patients being discharged with resources and hotlines. One example is Caring Contact.
Caring Contact is a crisis hotline and listening community for individuals in crisis, as well as a training opportunity for first responders and other members of the community. Caring Contact partners with the Crisis Text Line and the National Suicide Prevention Lifeline.
Training Resources
It is known that EDs often have a shortage of mental health professionals. If a hospital is not able to increase the number of mental health professional in the ED, it is crucial that emergency medical professionals receive training in managing psychiatric emergencies such as suicide crises.
Providers in the ED have the training and skills to triage a wide variety of physical conditions using risk-stratification techniques. Not all patients need to be referred to a specialist within or outside of the ED, and providers need to be confident in their ability to triage patients at risk for suicide the same as they are for physical conditions.
References
- https://www.sprc.org/settings/emergency-departments
- Knesper, D. J. (2010). Continuity of care for suicide prevention and research: Suicide attempts and suicide deaths subsequent to discharge from the emergency department or psychiatry inpatient unit. Newton, MA: Suicide Prevention Resource Center.
- Ahmedani, B. K., Simon, G. E., Stewart, C., Beck, A., Waitzfelder, B. E., Rossom, R., . . . Solberg, L. I. (2014). Health care contacts in the year before suicide death. Journal of General Internal Medicine, 29(6), 870–877.
- https://jamanetwork.com/journals/jamapsychiatry/fullarticle/2623157
- Montana Office of Epidemiology and Scientific Support, 2018. Montana Hospital Discharge Data system analysis by Cody Custis
- IBID and the Centers for Disease Control and Prevention.
- https://leg.mt.gov/content/Committees/Interim/2017-2018/Children-Family/Meetings/Sept-2018/sept2018-suicide-prevention-plan.pdf
- Coburn VA, Mycyk MB. Physical and chemical restraints. Emerg Med Clin North Am. 2009;27:655-667, ix.
- Ilgen MA, Walton MA, Cunningham RM, et al. Recent suicidal ideation among patients in an inner city emergency department. Suicide Life Threat Behav. 2009;39:508-517.
- Capoccia L, Labre M. Caring for Adult Patients With Suicide Risk: A Consensus-Based Guide for Emergency Departments. Waltham, MA: Education Development Center, Inc, Suicide Resource Prevention Center; 2015. Available at: http://www.sprc.org/ed-guide. Accessed July 23, 2015.

