Addressing Suicide in the Older Population
Introduction
Older adults are now and will continue to be the fastest growing segment of the population in the United States. The U.S. Census projects that more than 20% of the U.S. population, almost 73 million adults, will be 65 or older by the year 2030. 1 Research has shown that older adults have the highest rate of suicide compared to any other group. Additionally, older adults are more likely to die from a suicide attempt for a number of reasons, including being less likely to be found, more likely to plan carefully and use more deadly methods, and are more physically frail making them less liked to recover from a suicide attempt. 1 out of every 4 older adults who attempt suicide dies, compared to 1 out of every 100–200 younger adults who attempt suicide. 2 Suicide rates are particularly high among older men, especially those over 85 years of age. Men are more likely to use more lethal means, such as firearms, which could attribute to their increased likelihood of suicide attempt resulting in death.
Suicide Care Pathway
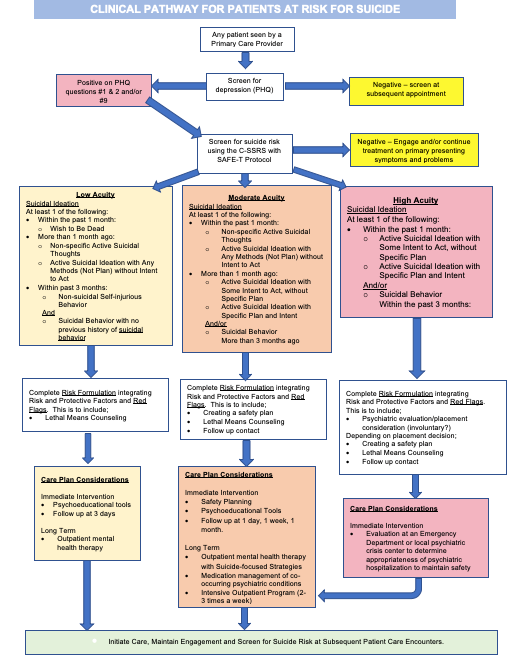
Text Version
Risk and Protective Factors
Risk Factors
- Previous suicide attempt
- Comorbid physical health conditions
- Depression and other mental health problems
- Social isolation
- Disability and pain
- Substance use problems (including abuse of prescription medications)
- Stressful life events and loss
- Access to lethal means
- Finding it difficult to adjust to change
Protective Factors
- Assessment and care for physical and mental health conditions
- Social connectedness
- Skills in coping and adapting to change
- A sense of purpose and meaning
- Participation in community activities
IS PATH WARM?
“IS PATH WARM” is an easy-to-remember mnemonic for the warning sides of suicide. It was created by the American Association of Suicidology to help counselors and the general public remember the warning signs of suicide.
| I | Ideation | Thoughts of suicide (expressed, threatened, written). |
|---|---|---|
| S | Substance Use | Increased or excessive alcohol or drug use. |
| P | Purposelessness | Seeing no reason for living, having no sense of meaning or purpose in life. |
| A | Anxiety | Anxiousness, agitation, nightmares, inability to sleep or excessive sleeping. |
| T | Trapped | Feeling as though there is no way out of current circumstances |
| H | Hopeless | Feeling hopeless about oneself, others or the future. |
| W | Withdrawal | Isolation from friends, family, usual activities, society. |
| A | Anger | Feelings of rage or uncontrollable anger, seeking revenge for perceived wrongs. |
| R | Recklessness | Acting without regard for consequences, excessively risky behavior. |
| M | Mood Changes | Dramatic changes in mood, unstable mood. |
Training
Training for those who serve older adults is typically focused on physical health needs, but data has shown that addressing suicide risk among older adults is becoming more crucial every year. There are a variety of training programs available both online and in person to prepare staff, caregivers, and lay people in the community to help recognize suicide risk and implement prevention and treatment strategies among older adults.
Question, Persuade, and Refer (QPR)
QPR Institute provides several trainings for professionals and lay people in recognizing and responding effectively to someone showing suicide warning signs and behaviors. An initial Gatekeeper training is available online and the QPR intervention has been used successfully on older adults. In addition to the general gatekeeper training, there are a number of other trainings available on the QPR Institute website, including “QPR for Eldercare Workers,” which includes specific recommendations and insights for suicide prevention among older adults.
- Training: QPR for Eldercare Workers
Applied Suicide Intervention Skills Training (ASIST)
ASIST is an interactive, practice-oriented workshop that teaches first aid to caregivers with a focus on encouraging help-seeking in at-risk individuals. This training is designed for any caregivers of older adults, including paraprofessionals, professionals, and lay people. Those trained learn how to prevent suicide by recognizing warning signs, providing intervention, and developing a safety plan.
Recognizing and Responding to Suicide Risk: Essential Skills for Clinicians (RRSR)
RRSR is a longer, two-day training created by the American Association of Suicidology (AAS) with a focus on training mental health professionals who work with older adults. The training is based on the 24 core competencies of the AMSR training described below. It allows mental health clinicians to practice learned skills through case application exercises.
Assessing and Managing Suicide Risk: Core Competencies for Mental Health Professionals (AMSR)
The Suicide Prevention Resource Center (SPRC) and American Association of Suicidology (AAS) created the ASMR training as a one-day workshop based on 24 core competencies that came from a consensus process among leading clinicians and researchers. These competencies are aimed at effectively assessing and managing suicide risk and the audience of the training is typically mental health professionals.
Screening
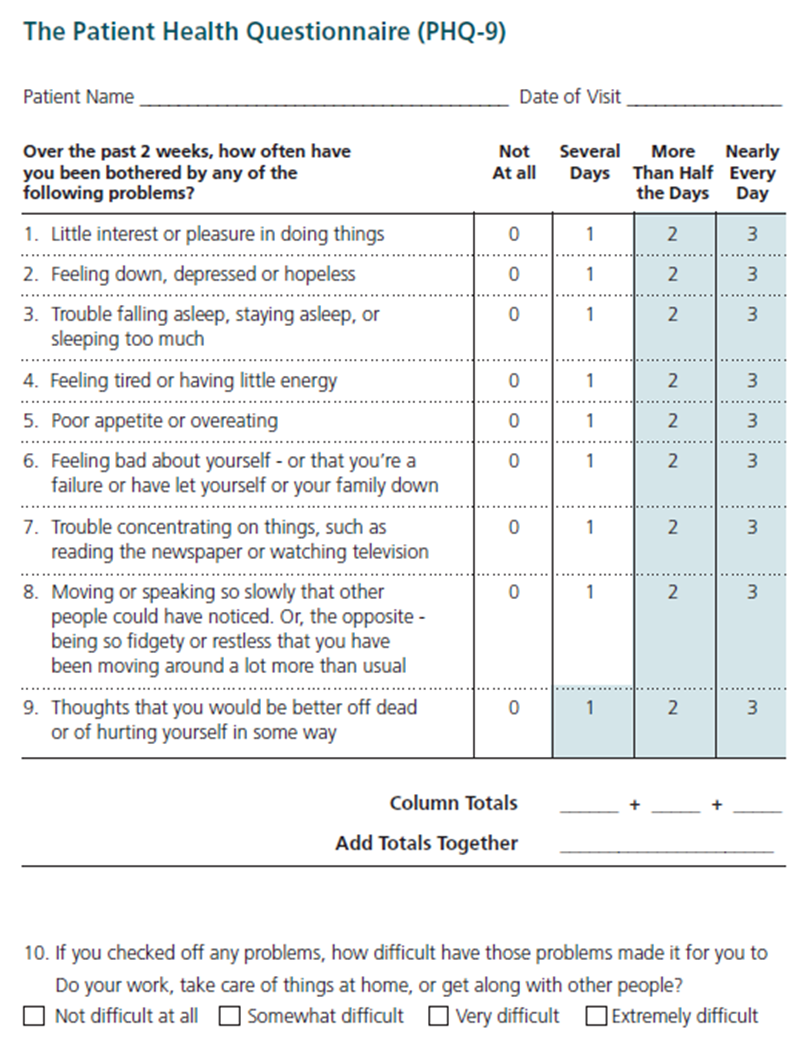
Patient Health Questionnaire-9 (PHQ-9): The PHQ-9 is a self-administered (but can be clinician-administered) screening tool for depression that has a specific question (Question #9) regarding suicide. The PHQ-9 is scored from 0 (not at all) to 3 (nearly every day). The PHQ-9 is shorter than other scales, can be administered in person, by telephone, or self-administered, facilitates diagnosis, provides assessment of symptom severity, is validated in a variety of populations, and can be used in adolescents as young as 12 years old. 3 Question #9 specifically asks whether respondents have “thoughts that you would be better off dead or of hurting yourself in some way.” Regardless of the total score, a positive response to question # 9 warrants further risk assessment.
| Severity Levels | PHQ-9 score |
|---|---|
| Normal | 0 - 4 |
| Mild | 5 - 9 |
| Moderate | 10 - 14 |
| Moderate to severe | 15 - 19 |
| Severe | 20 - 27 |
This tool has been validated for its use in primary care settings and can be a critical tool in assisting primary care providers in diagnosing depression and suicide risk and monitoring treatment response. 4
- One study found that those who answered “nearly every day” to question 9 on the PHQ-9 had a 4% probability of suicide attempt in the following year, a ten-fold increase compared to .04% of those who answered “not at all.” 5
- Another large study found that those who score positive on Question #9 of the PHQ-9 were 5 to 8 times more likely to attempt suicide and 3 to 11 times more likely to die by suicide within 30 days, and were 2 to 4 times more likely to attempt suicide and 2 to 6 times more likely to die by suicide within a year. This increased risk persisted for two years. 6
This data shows that suicidal ideation reported on the PHQ-9 is a robust indicator of suicide attempts and deaths, demonstrating the need for providers and healthcare systems to address immediate and sustained risk for suicide in patients who screen positive on the PHQ-9. 7
Beck Scale for Suicide Ideation (BSI): The BSI is a 21-item self-report instrument for detecting and measuring the current intensity of the patients’ specific attitudes, behaviors, and plans to commit suicide during the past week.
Geriatric Depression Scale (GDS): The GDS comes in both long-form (30 questions) and short-form (15 questions) and asks participants to respond by answering yes or no in reference to how they felt over the past week. Questions include items such as mood, life satisfaction, energy, and activity level.
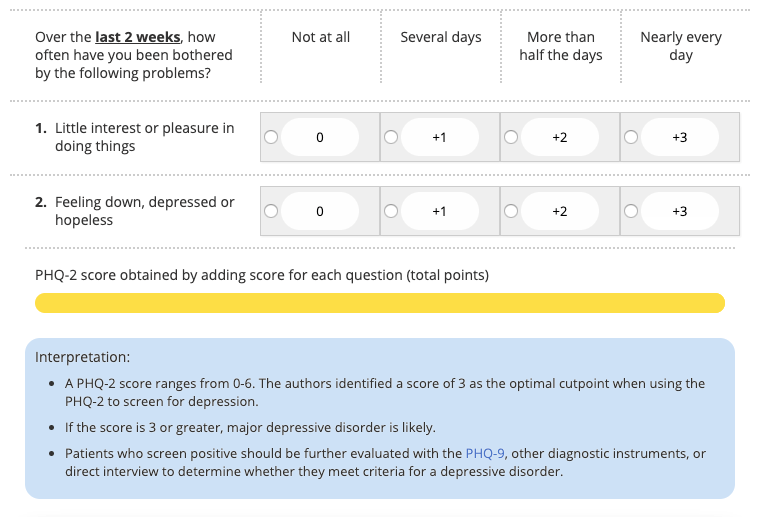
Patient Health Questionnaire-2 (PHQ-2): The PHQ-2 includes two questions (the first two questions from the PHQ-9) to inquire about the frequency of depressed mood over the last two weeks. This is a “first-step” approach, and all patients who screen positive should be further evaluated using the PHQ-9.
Columbia-Suicide Severity Rating Scale (C-SSRS): This tool can be used to both screen and assess suicide risk. The C-SSRS is utilized to identify whether the patient has thought about suicide, has taken action or plans to take action, or whether they attempted suicide or plan to attempt suicide. The questionnaire begins with two questions about passive or active suicidal ideations, leading to further follow up questions based on positive responses to gauge severity. Based on the severity, resources are available with interventions for responding to the C-SSRS. This tool has an expansive evidence base and is supported by SAMHSA, the CDC, the FDA, the NIH, the WHO, and many others. The tool is scored as Low, Moderate or High risk, depending on positive answers. The most concerning answers include: a recent (past month) “yes” to question 4 or 5 (shown below) on ideation severity and/or any recent (past 3 months) behavior.
- An extra benefit of the C-SSRS is built-in triage guidelines. It contains a comprehensive guide to using the scale for triage in a clinical setting.
- While the C-SSRS is unique in that it can be used by healthcare professionals, as well as friends, families, and individuals in the community, training staff to use the C-SSRS and all screening tools is important in increasing their comfort level and sense of competence. Training resources both online or in-person.
|
Ask questions that are bold and italicized. |
Past month |
|
|---|---|---|
|
Ask Questions 1 and 2 |
YES |
NO |
|
1) Have you wished you were dead or wished you could go to sleep and not wake up? |
|
|
|
2) Have you had any actual thoughts of killing yourself? |
|
|
|
If YES to 2, ask questions 3, 4, 5, and 6. If NO to 2, go directly to question 6. |
||
|
3) Have you been thinking about how you might do this? e.g. “ I thought about taking an overdose but I never made a specific plan as to when where or how I would actually do it….and I would never go through with it.” |
|
|
|
4) Have you had these thoughts and had some intention of acting on them? as opposed to “ I have the thoughts but I definitely will not do anything about them.” |
|
|
|
5) Have you started to work out or worked out the details of how to kill yourself? Do you intend to carry out this plan? |
|
|
|
6) Have you ever done anything, started to do anything, or prepared to do anything to end your life? Examples: Collected pills, obtained a gun, gave away valuables, wrote a will or suicide note, took out pills but didn’t swallow any, held a gun but changed your mind or it was grabbed from your hand, went to the roof but didn’t jump; or actually took pills, tried to shoot yourself, cut yourself, tried to hang yourself, etc.
|
Lifetime |
|
|
|
|
|
|
Past 3 Months |
||
|
|
|
|
Response Protocol to C-SSRS Screening
Item 1 - YELLOW - Behavioral Health Referral
Item 2 - YELLOW - Behavioral Health Referral
Item 3 - ORANGE - Behavior Health Consult (Psychiatric Nurse/Social Worker) and consider Patient Safety Precautions
Item 4 - RED - Behavioral Health Consultation and Patient Safety Precautions
Item 5 - ORANGE - Behavior Health Consult (Psychiatric Nurse/Social Worker) and consider Patient Safety Precautions
Item 6 - 3 months ago or less - RED - Behavioral Health Consultation and Patient Safety Precautions
Suicide Assessment Five-Step Evaluation and Triage (SAFE-T): Typically found in the form of the SAFE-T Protocol Card, SAFE-T is a 5-step suicide assessment protocol used to address a patient’s level of suicide risk and suggest appropriate interventions. A detailed guide for the 5 steps, with specific language and scripts, can be found here: SAFE-T Quick Guide for Clinicians.
Interventions
Healthy IDEAS (Identifying Depression, Empowering Activities for Seniors)
This program detects and reduces the severity of depression in older adults with chronic health problems and functional limitations. It integrates four evidence-based components into the regular services provided to older adults in their homes. It uses screening, education of clients and family, referral and linkage to mental health services, and behavioral activation.
The Program to Encourage Active and Rewarding Lives for Seniors (PEARLS)
The PEARLS program uses problem-solving therapy, tools and strategies to increase social and physical activities, and strategies to focus on pleasant events to reduce depression in physically impaired and socially isolated older adults. PEARLS is designed for older adults with minor depression or dysthymia.
Telephone-Based Programs
Some community-based programs use the telephone as their main form of contact with older adults. Senior living communities might consider using this type of model in their community or look to see if a similar type of program exists in their area.
- Link-Plus: A social work service with case management provided over the phone under auspices of the suicide prevention hotline agency, Life Crisis, Inc. Link-Plus targets older adults at risk for suicide and provides multidimensional assessment, service arrangement (case management), and supportive therapy.
- TeleHelp - Telecheck: Provides older adults living at home with support. TeleHelp is referred to as an “alarm system,” with which a senior in crisis can activate a call for help. In TeleCheck, the client is contacted twice weekly by telephone for assessment of needs and emotional support. This program has been proven especially useful in rural areas and is run in some areas by churches.
- Older Adults - Suicide Prevention Alliance: provides useful resources and support for seniors, caregivers and the general public.
988: Provides free and confidential emotional support to people in suicidal crisis or emotional distress, 24 hours a day, 7 days a week, across Montana.

Friendship Line: The Friendship Line was created by the Institute on Aging, Center for Elderly Suicide Prevention for professionals in mental health and aging to provide to consumers. Description: This program offers a range of services, including a 24-hour crisis and support hotline, outreach calls to seniors for emotional support, home visits for counseling and psychotherapy, bereavement counseling, support groups, online mental health screening, and education on suicide intervention.
Lethal Means Restriction: Anyone who is identified with any level of suicide risk, from mild to severe, should be asked about access to lethal means. Removing access to lethal means for individuals at risk for suicide should be a top priority, as research shows that over 50% of suicides are completed using a firearms. 8 In the last decade, the majority of suicide deaths (approximately 70%) among older adults were linked to firearms, with men accounting for more than 90% of those deaths. Other common lethal means used by older adults include poisoning and suffocation.
In Montana, firearms were used in 63% of suicides in 2016. 9 Providers and patients should discuss and monitor other lethal means as well, such as access to materials for hanging/suffocation (belts, ropes, or other items) or large quantities of high-risk medications.
Counseling on Access to Lethal Means (CALM): CALM is a workshop that helps providers identify patients who would benefit from lethal means counseling strategies, ask about access to lethal means, and work with patients and their family to reduce access. 10 More information and guidance about which patients need counseling on access to lethal means
- CALM workshop
- For Clinicians : Sample language and steps, goals, and things to consider when talking with patients about reducing access to lethal means.
- What Clients and Families Need to Know
- Basics of Firearms
- Firearms Laws Relevant to Lethal Means Counseling
Suicide Safety Planning: Much like action plans for physical illnesses, creating a Suicide Safety Plan can be useful for patients to refer to during moments of distress. Suicide Safety Planning is evidence-based and can help patients manage suicidal thoughts and reduce emergency rooms visits. Safety Plans are created by the patient in conjunction with a provider. Safety Plans include identifying triggers and warning signs, specific activities that can steer the patient from suicidal thoughts, contacts to be used during times of distress (community, professional, and emergency), etc.
- Training for staff on how to create a safety plan
- Suicide Safety Planning Quick Guide
- NowMattersNow Comprehensive Safety Plan Guide
- Safety Plan pdf
Suicide Prevention Resources (trainings and programs)
- QPR - A two-hour gatekeeper training that provides anybody the ability to recognize the warning signs, how to intervene, and who to refer the person to.
- ASIST - A two-day workshop designed to provide participants with gatekeeping knowledge and skills. Gatekeepers are taught to recognize the warning signs and to intervene with appropriate assistance.
- Mental Health First Aid - Mental Health First Aid is an adult public education program designed to improve participants' knowledge and modify their attitudes and perceptions about mental health and related issues, including how to respond to individuals who are experiencing one or more acute mental health crises or are in the early stages of one or more chronic mental health problems. There is now a specialized version of MHFA that focuses on older adults.
More Resources
For Senior Living Communities: Senior living communities include organizations such as nursing homes, assisted living facilities, independent living facilities and continuing care retirement communities.
- Toolkit: Promoting Emotional Health and Preventing Suicide for Senior Centers This toolkit contains items such as:
- Sample Policy template
- Facility assessment checklist
- List of activities to engage every member of the population served in promoting emotional well-being
- Strategies to reduce access to lethal means
- Making connections with community mental health providers
- A template for Crisis Response protocols, for Responding to a Suicide Death, Postvention after a Suicide Death, and Communicating with Residents, Families, Staff, and the Media.
- Information Sheet on The Role of Senior Living Community Professionals in Preventing Suicide
For Senior Centers: Senior Centers can vary in size, location, population services, funding sources, staffing, services, and activities, as well as their approaches to mental health promotion and suicide prevention.
- Promote emotional health: Activities that promote emotional wellbeing should focus on all older adults in care, not just those at risk for suicide. The activities include a range of programs and services that support emotional health and help older adults develop positive social connections. Some examples include sessions on topics such as diabetes management and injury prevention, workshops on issues such as loss, volunteering and mentoring opportunities, word and number games, cooking, using computers, etc.
- Recognize and respond to suicide risk: Senior Center Staff typically spend time with older adults daily, placing them in a unique position to notice signs of a problem and encourage help-seeking behavior. They can also identify older adults who may be at risk for suicide and related mental health and substance use disorders and link them to sources of help. Senior Centers can designate someone at their facility as a point person for addressing concerns related to suicide risk, can connect older adults to a mental health professional in the community if there is not one on staff, and develop a protocol for recognize and immediately respond to suicide warning signs, and provide training for staff, volunteers, and older adults.
- Respond to a suicide attempt or death: A suicide attempt or death can have a profound emotional effect on older adults, caregivers, senior care staff, and volunteers.
For Primary Care Providers: Please see section on primary care intervention
Additional Resources
Suicide Prevention for Older Adults
This booklet, intended for use by healthcare providers, lists risk factors for suicide and a few statistics on suicide in older adults. It summarizes studies that show effectiveness in preventing suicide, including treatment for depression. It also lists goals and objectives from the National Suicide Prevention Strategy that address suicide prevention in older adults.
Assessing Suicide Risk: Initial Tips for Counselors
This wallet card can be used by counselors and other health care professionals. The card describes initial steps to take when you think a person may be suicidal. It also includes the Lifeline phone number.
Elderly Suicide Fact Sheet
This fact sheet presents statistics on elderly suicide deaths; by age, gender, race, and means. It includes the role of depression, substance abuse, and other common risk factors.
Late Life Suicide Prevention Toolkit: Life Saving Tools for Health Care Providers
These training materials include an interactive, case-based DVD, the National Guidelines for Seniors’ Mental Health: The Assessment of Suicide Risk and Prevention of Suicide; a clinician pocket card, a facilitator’s guide, and a PowerPoint presentation.
Get Connected: Linking Older Adults with Medication, Alcohol, and Mental Health
This toolkit is designed to assist program managers with planning prevention programs to address substance use and mental health problems in older adults. It covers assessing the readiness of an organization to implement a program, creating an arsenal of resources as sources of information, planning staff education, and writing a program plan. The toolkit is accompanied by a booklet that profiles program success stories.
References
- Ortman, J. M., Velkoff, V. A., & Hogan, H. (2014). An aging nation: The older population in the United States. Retrieved from www.census.gov/prod/2014pubs/p25-1140.pdf
- (American Association of Suicidology, 2009)
- https://aims.uw.edu/resource-library/phq-9-depression-scale
- https://pubmed.ncbi.nlm.nih.gov/18186994/?dopt=Abstract
- https://ps.psychiatryonline.org/doi/full/10.1176/appi.ps.201200587
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5412508/
- https://www.sprc.org/scope/means-suicide
- https://sprc.org/wp-content/uploads/2022/12/2016-Montana-Suicide-Mortality-Review-Report.pdf
- https://sprc.org/online-library/calm-counseling-on-access-to-lethal-means/

