Suicide Prevention in Pediatric Populations
Introduction
Suicide is the 2nd leading cause of death for individuals age 10-18 years, second only to unintentional injury.1 The number of encounters at children’s hospitals for suicidal ideation or suicide attempt among school-aged children and adolescents has more than doubled since 2008.2
- 17% of youth in grades 9-12 seriously considered suicide in the previous 12 months and 8% made one or more attempts within the same time period.3
- Rural youth are at particularly high risk of suicide, with suicide rates approximately double those in urban areas.4
- Firearms remain the most common means of death, however, death by suffocation, particularly hanging, is nearly as common and is the leading cause of death by suicide in children under 12.5,6
- In general, youth with frequent and severe suicidal ideation (i.e., high levels of intent and/or planning) have about a 60% chance of making a suicide attempt within 1 year of ideation onset.7
Over the past ten years, Montana has had a youth suicide rate double the national rate.
2009 - 2018, United States
Suicide Injury Deaths and Rates per 100,000
All Races, Both Sexes, Ages 10 to 17
ICD-10 Codes: X60-X84, Y87.0,*U03
| Number of Deaths | Population*** | Crude Rate |
|---|---|---|
| 13,445 | 333,676,326 | 4.03 |
2009 - 2018, Montana
Suicide Injury Deaths and Rates per 100,000
All Races, Both Sexes, Ages 10 to 17
ICD-10 Codes: X60-X84, Y87.0,*U03
| Number of Deaths | Population*** | Crude Rate |
|---|---|---|
| 97 | 1,007,300 | 9.63 |
Some psychological factors are significantly greater among children at risk for suicide compares that those without suicide risk, including hopelessness, low self-esteem, external locus of control, and problems regulating anger.8
Risk Factors and Warning Signs for Suicide Among Youth
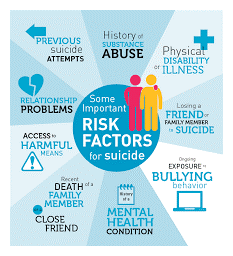
There are several risk factors for suicide among children and teens, including:
- previous suicide attempts, suicidal ideation, family history of suicide
- isolation, loneliness, feeling trapped, withdrawal, hopelessness, limited ability to identify reasons for living, limited or no sense of belonging, feeling like a burden
- psychiatric conditions and mental conditions (anxiety, depression, conduct disorders, substance abuse/dependence)
- medical conditions/pain
- childhood maltreatment or trauma, family stress/dysfunction, family violence
- relationships with peers, bullying and harassment
- limited coping skills
- mood changes, recklessness, changes in sleeping habits, changes in eating habits, giving away prized possessions
- unstable psychosocial and social stressors
- losses (breakup, academic failure, trouble with authorities/serious disciplinary action, death of a loved one)
- self-injury
More detailed list of subtle warning signs for suicide in children.
Co-Morbidities Among Children
Suicidality among children and adolescents with Bipolar Disorder: Risk for completed suicide by individuals with bipolar disorder is among the highest of all psychological disorders.9 Given that suicidality is so common among patients with bipolar disorder, providers should regularly screen and assess all patients in their care with bipolar disorder for suicide risk. More information on risk factors, assessment, and treatment
ADD/ADHD and Suicidality: Children with ADHD are at a higher risk of developing psychiatric disorders such as substance use disorders, depression, and antisocial behavior.11 Research also shows that impulsivity and aggression are traits often seen among individuals with ADHD, and they are also common among those experiencing suicidal thoughts or behaviors. For this reason, providers should consider suicide screening of children and adolescents with ADHD.11
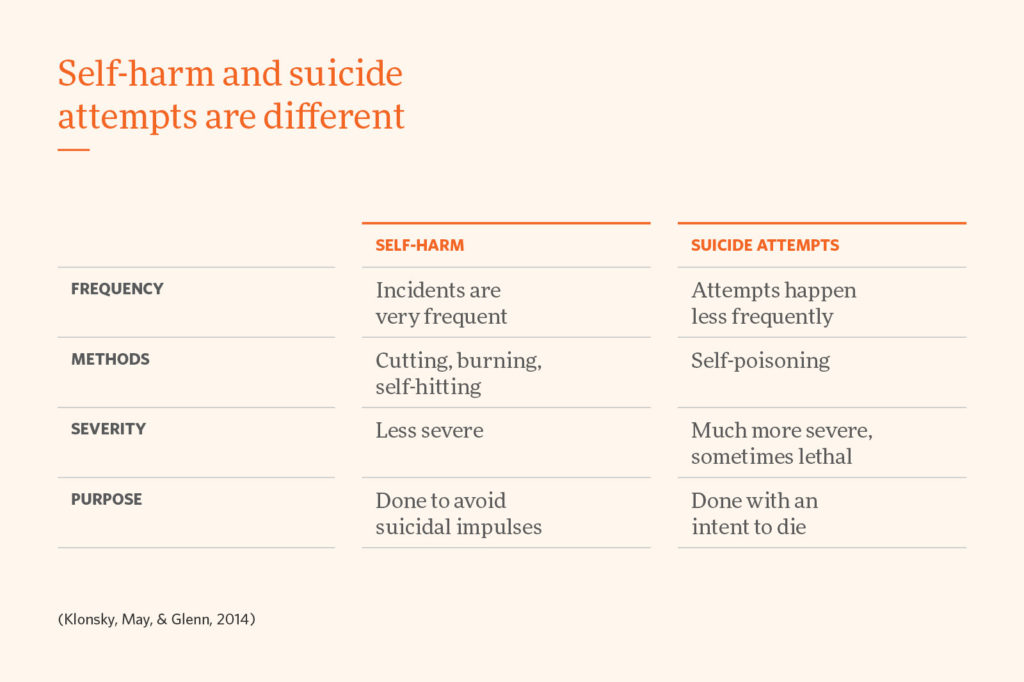
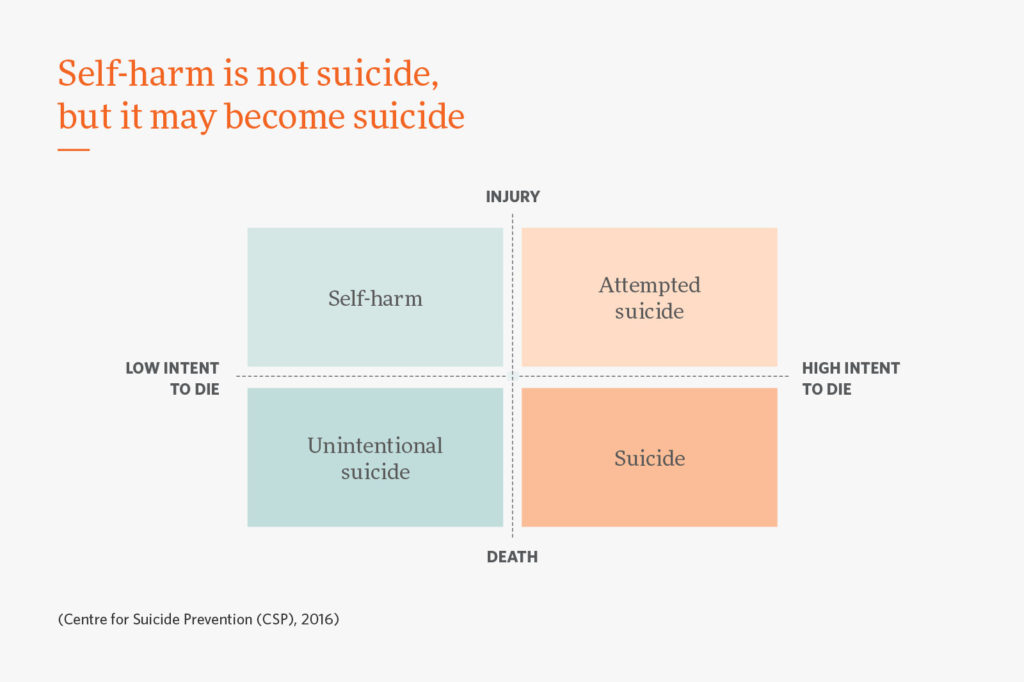
Self-Injurious Behaviors and Suicide: Self-injurious behavior affects between 13-45% of young people and includes cutting, burning or hitting oneself, scratching to the point of bleeding, or interfering with healing.12
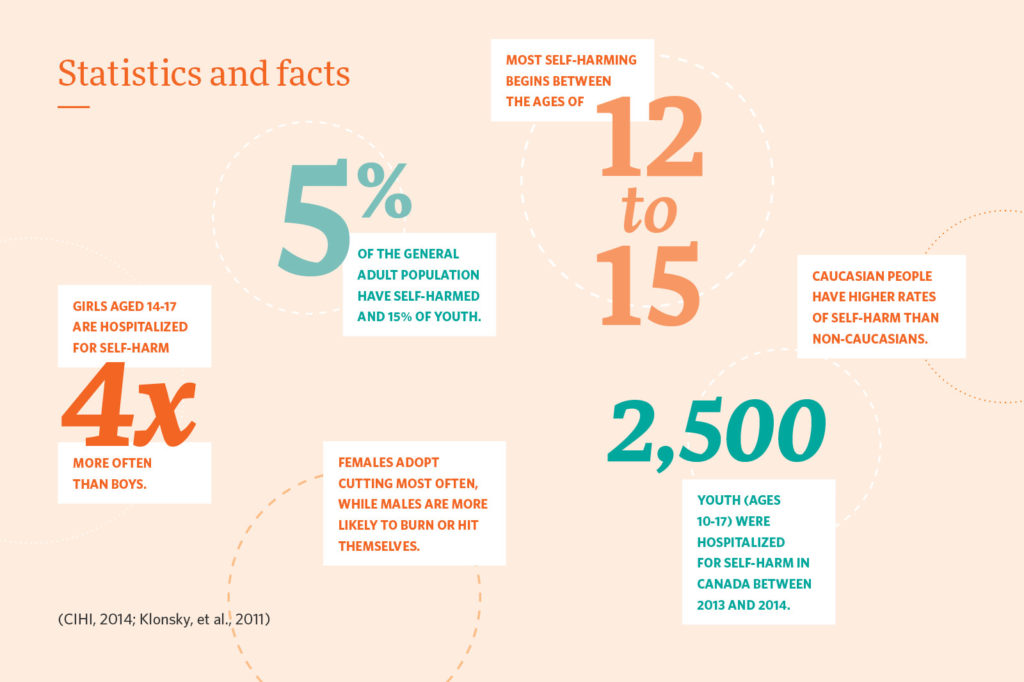
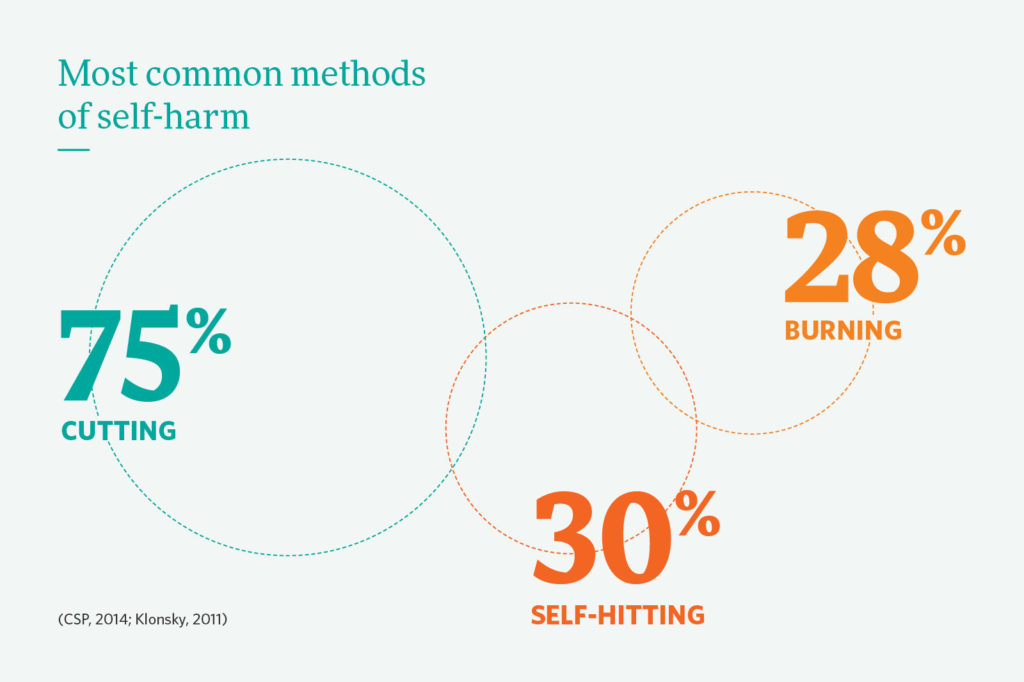
This behavior can be used to reduce or regulate negative emotions, but it can also be a factor that precipitates suicidal ideation or attempts. Among those with a history of self-injurious behaviors, 70% have attempted suicide at least once and 55% several times.13 While self-injurious behavior has not been proven as a direct risk factor for suicide, this behavior regularly co-occurs with suicidality.
There are a wide variety of terms associated with self-injurious behaviors, such as self-harm, self-abuse, self-mutilation, non-suicidal self-injury, deliberate self-harm, etc. This had led to confusion in both research and clinical settings. Some studies have concluded that less than half of those who self-injure have made at least one suicide attempt, and that self-injurious behavior can escalate into suicidal behavior.14 Self- injury is particularly dangerous because individuals can reach a point where self-injury is no longer working as an effective coping mechanism for them to offset negative emotions or an individual may become desensitized or habituated to pain and may view suicide as less frightening.14
- A great resource for warning signs, what to say to patients who self-injure, treatments, and data
- S.A.F.E (Self Abuse Finally Ends): Provides outpatient services to individuals who want to self-injure and want to stop.
- S.I.O.S (Self-Injury Outreach and Support): This website is a helpful resource about self-injury, including information guides for individuals, friends, romantic partners, school professionals, mental health and medical professionals.
References:
- https://www.nimh.nih.gov/health/statistics/suicide.shtml
- https://pediatrics.aappublications.org/content/141/6/e20172426
- CDC. 2017 Youth Risk Behavior Survey Questionnaire (YRBSS). www.cdc.gov/yrbs. Accessed
- Fontanella CA, Hiance-Steelesmith DL, Phillips GS, et al. Widening rural-urban disparities in youth suicides, United States, 1996-2010. JAMA Pediatr. 2015;169(5):466-473
- CDC. Web-based Injury Statistics Query and Reporting System (WISQARS). (2018) Atlanta, GA: National Center for Injury Prevention and Control. https://www.cdc.gov/injury/wisqars/index.html. Accessed.
- Sheftall AH, Asti L, Horowitz LM, et al. Suicide in elementary school-aged children and early adolescents. Pediatrics. 2016;138(4):e20160436.
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2827306/#R40
- https://www.sciencedirect.com/science/article/abs/pii/S0165032706000024
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2827306/
- Treatment guidelines for children and adolescents with bipolar disorder. Kowatch RA, Fristad M, Birmaher B, Wagner KD, Findling RL, Hellander M, Child Psychiatric Workgroup on Bipolar Disorder. J Am Acad Child Adolesc Psychiatry. 2005 Mar; 44(3):213-35.
- James, A., Lai, F. H., & Dahl, C. (2004). Attention deficit hyperactivity disorder and suicide: a review of possible associations. Acta Psychiatrica Scandinavica, 110(6), 408–415
- https://chadd.org/attention-article/adhd-self-harm-and-suicide/
- Hargus E, Hawton K, Rodham K. Distinguishing Between Subgroups of Adolescents Who Self‐Harm. Suicide Life Threat Behav. 1 October 2009;39(5):518–37. 10.1521/suli.2009.39.5.518
- https://www.suicideinfo.ca/resource/self-harm-and-suicide/
Clinical Pathway for Patients at Risk for Suicide
In order to begin caring for patients who may be at risk for suicide, providers must take into account the patient’s history, current circumstances and presence of suicidal ideation, as well their combined risk and protective factors. Clinical pathways for patients at risk for suicide incorporate steps, goals, screening tools, care plan considerations, and maintenance. Clinical decisions regarding suicide should take into consideration the full range of factors to determine level, extent, and imminence of risk, which in turn informs the steps that need to be taken to increase safety and reduce risk. We expand here on evidence-based tools for screening and assessment, treatment interventions, and additional resources and links for training, research, and information.
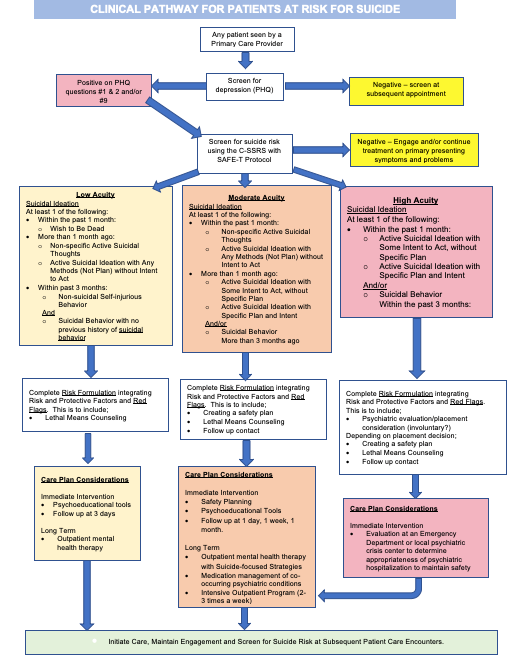
Screening
Early detection of suicide risk is crucial. Multiple studies demonstrate that one predictor of future suicidal behavior is past suicidal behavior,1 with a reattempt rate ranging from 6% to 15% per year and the greatest risk occurring within 3 months of the initial attempt.2
In recent years, Suicide Risk Screening has been recommended for all medical patients. This suicide risk screening should be incorporated into yearly well visits, and more frequently for patients with other behavioral health concerns (ADHD, anxiety, substance abuse) or trauma history. Improving screening implementation increases detection of suicide risk, without overburdening busy healthcare staff or systems. To maintain accurate detection of suicide risk in your population, it is important to use validated, evidence-based suicide risk screening tools. Research also shows that children and adolescents may be more likely to report suicidal ideation through self-administered scales rather than through face-to-face interviews.10 Additionally, children and adolescents may be more likely to disclose suicidality if a parent or guardian is not present.
Evidence Based Screening Tools
Pediatric Symptom Checklist (PSC): The Pediatric Symptom Checklist is a psychosocial screening tool designed to facilitate recognition of cognitive, emotional, and behavioral problems. There is a Parent-Completed version (PSC) and a Youth-Completed version (Y-PSC) for children ages 11 and up. This screener is used regularly in pediatric practices, and while not intended to identify suicide, this tool can help identify risk for suicide based on responses to the emotional and behavioral questions.
The PSC consists of 35 items that are rated as “Never,” “Sometimes,” or “Often” present and scored 0, 1, and 2, respectively. The total score is calculated by adding together the score for each of the 35 items.
- For children and adolescents ages 6 through 16, a cutoff score of 28 or higher indicates psychological impairment.
- For children ages 4 and 5, the PSC cutoff score is 24 or higher (Little et al., 1994; Pagano et al., 1996). The cutoff score for the Y-PSC is 30 or higher.
- Items that are left blank are simply ignored (i.e., score equals 0). If four or more items are left blank, the questionnaire is considered invalid.
- A positive score requires follow up by a mental health and health professional, to ensure proper interpretation and evaluation for false positives or negatives.
| No | Sometimes | Often | ||
|---|---|---|---|---|
| 01 | Complains of aches/pains without a physical cause | |||
| 02 | Spends more time alone | |||
| 03 | Tires easily | |||
| 04 | Fidgety, unable to sit still | |||
| 05 | Has trouble with teachers | |||
| 06 | Less interested in school | |||
| 07 | Acts as if driven by a motor | |||
| 08 | Daydreams too much | |||
| 09 | Distracted easily | |||
| 10 | Afraid of new situations | |||
| 11 | Feels sad, unhappy | |||
| 12 | Is irritable, angry | |||
| 13 | Feels hopeless | |||
| 14 | Has trouble concentrating | |||
| 15 | Less interest in friends | |||
| 16 | Fights with others | |||
| 17 | Absent from school | |||
| 18 | School grades dropping | |||
| 19 | Is down on him or herself | |||
| 20 | Visits doctor with doctor finding nothing wrong | |||
| 21 | Has trouble sleeping | |||
| 22 | Worries a lot | |||
| 23 | Wants to be with parents more than before | |||
| 24 | Feels he or she is bad | |||
| 25 | Takes unnecessary risks | |||
| 26 | Gets hurt frequently | |||
| 27 | Seems to be having less fun | |||
| 28 | Acts younger than children his or her age | |||
| 29 | Does not listen to rules | |||
| 30 | Does not show feelings | |||
| 31 | Does not understand other people's feelings | |||
| 32 | Teases others | |||
| 33 | Blames others for his or her troubles | |||
| 34 | Takes things that do not belong to him or her | |||
| 35 | Refuses to share | |||
PHQ-A (Patient Health Questionnaire-A): The PHQ-9 is an evidence-based screening tool for depression that has been modified for different populations. For children ages 11-17, the PHQ-A is used as an adaptation to the PHQ-9 for Adolescents. This tool screens broadly for depression (a risk factor for suicide) and self-harm and can be easily built into the EHR.
- Scored on a scale of 0-27
- Question #9 specifically asks whether they have "thoughts that you would be better off dead or of hurting yourself in some way." Regardless of the total score, a positive response to question #9 warrants further risk assessment.
Sample PHQ-A:
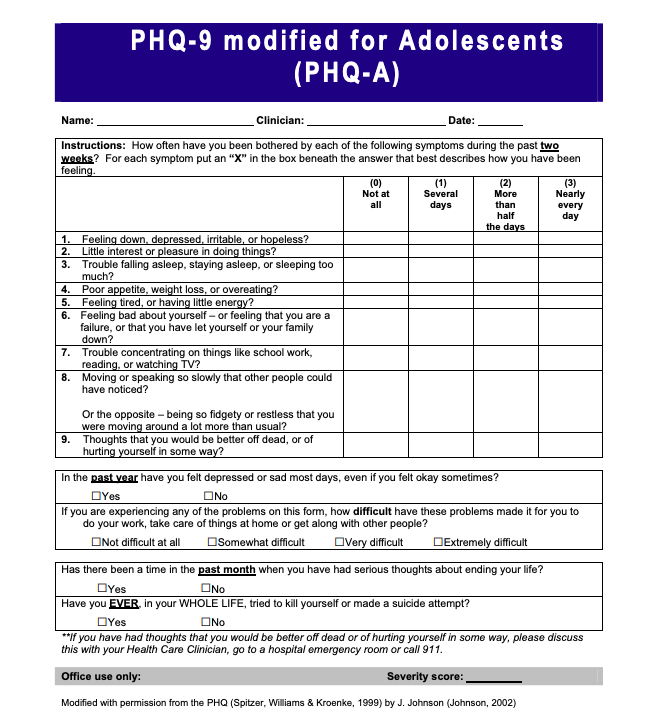
If suicide risk is identified during the PHQ-A, further assessment can be completed using another tool, such as the C-SSRS or the ASQ.
Assessment
If a patient screens positive for suicide risk during initial screening, further follow-up should be conducted by a provider or a mental health clinician. Assessment helps identify whether patients are imminent risk, high risk, or lower risk. Brief assessment using the C-SSRS or the ASQ can help providers determine the best next steps for the patient.
Columbia Suicide Severity Rating Scale (C-SSRS): This tool can be used to both screen and assess suicide risk. Originally created as part of a study on decreasing suicide risk among adolescents, the C-SSRS can be used on all patients over the age of 11. The C-SSRS is utilized to identify whether the patient has thought about suicide, has acted or plans to act, or whether they attempted suicide or plan to attempt suicide. The questionnaire begins with two questions about passive or active suicidal ideations, leading to further follow up questions based on positive responses to gauge severity. Based on the severity, resources are available with interventions for responding to the C-SSRS. This tool has an expansive evidence base, and is supported by SAMHSA, the CDC, the FDA, the NIH, the WHO, and many others. The tool is scored as Low, Moderate or High risk, depending on positive answers. The most concerning answers include: a recent (past month) “yes” to question 4 or 5 on ideation severity and/or any recent (past 3 months) behavior.
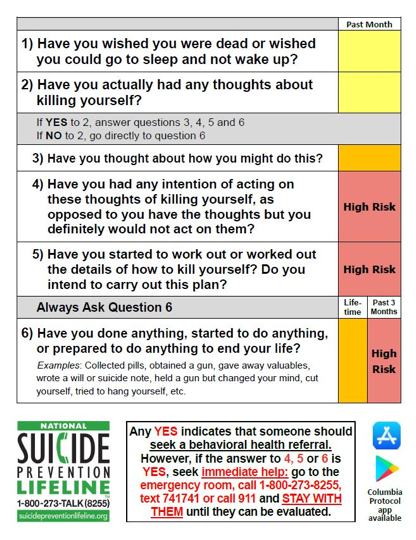
- An extra benefit of the C-SSRS is built-in triage guidelines. Comprehensive guide to using the scale for triage in a clinical setting.
- While the C-SSRS is unique in that it can be used by healthcare professionals, as well as friends, families, and individuals in the community, training staff to use the C-SSRS and all screening tools is important in increasing their comfort level and sense of competence. Training resources both online or in-person
- C-SSRS pdf
References
- onlinelibrary.wiley.com/doi/abs/10.1111/j.1399-5618.2007.00553.x
- www.sciencedirect.com/science/article/abs/pii/S0890856709631750
Ask Suicide-Screening Questions (ASQ): The ASQ is a brief questionnaire containing 4 items and can be utilized in all populations and practice settings (ED, inpatient medical, primary care settings). The tool is scored based on the “yes” or “no” answers, with a 5th question to assess “acuity.”
Sample ASQ:
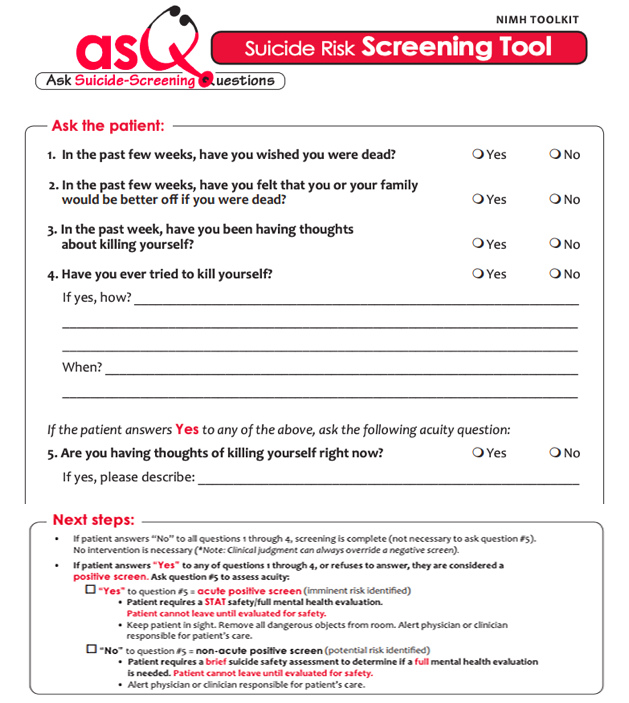
- A full ASQ toolkit is available from the National Institute of Mental Health, which includes access to the tool, information sheets, clinical pathways, and medical setting-specific resources.
- ASQ pdf
- ASQ information sheet
Treatment
After screening and assessment for suicide risk, a treatment plan should be developed when determined necessary. This should be completed by a mental health professional, whether embedded in your practice setting or by referral. Evidence base is growing for many interventions that address suicide risk, including Lethal Means Restriction, Safety Planning, Therapy, sometimes medication or psychiatric consultation, and sometimes even Crisis Referral.
Lethal Means Restriction:
Anyone who is identified with any level of suicide risk, from mild to severe, should be asked about access to lethal means. Research shows that firearms are the primary method used in teen suicides, while in elementary-school aged children, hanging is used most often.1 Removing access to lethal means for individuals at risk for suicide should be a top priority for the patient’s family or guardians, as research shows that 80% of guns used in youth suicide belonged to a parent.2 Parents or guardians of the patient should monitor other lethal means as well, such as access to materials for hanging/suffocation (belts, ropes, or other items) or large quantities of high-risk medications.
Counseling on Access to Lethal Means (CALM): CALM is a workshop that helps providers identify patients who would benefit from lethal means counseling strategies, ask about access to lethal means, and work with patients and their family to reduce access.3 More information and guidance about which patients need counseling on access to lethal means
- Workshop
- For Clinicians: Sample language and steps, goals, and things to consider when talking with patients about reducing access to lethal means.
- What Clients and Families Need to Know
- Basics of Firearms
- Firearms Laws Relevant to Lethal Means Counseling
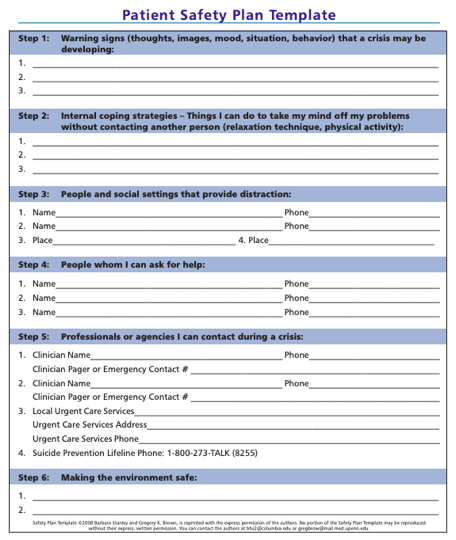
Suicide Safety Planning: Much like action plans for physical illnesses, creating a Suicide Safety Plan can be useful for patients to refer to during moments of distress. Suicide Safety Planning is evidence-based and can help children and teens manage suicidal thoughts and reduce emergency rooms visits. Safety Plans are created by the child or teen in conjunction with a provider. Safety Plans include identification of triggers and warning signs, specific activities that can steer the patient from suicidal thoughts, contacts to be used during times of distress (community, professional, and emergency), etc.
- Sheftall AH, Asti L, Horowitz LM, et al. Suicide in elementary school-aged children and early adolescents. Pediatrics. 2016;138(4):e20160436.
- Azrael D, Cohen J, Salhi C, Miller M. Firearm Storage in Gun-Owning Households with Children: Results of a 2015 National Survey. J Urban Health. 2018;95(3):295-304.
- https://sprc.org/online-library/calm-counseling-on-access-to-lethal-means/

