Addressing Suicide in OB/GYN Settings
Obstetricians and Gynecologists (OB/GYNs) specialize in women’s health, from reproductive health to pregnancy, childbirth, post-partum and throughout the life cycle. There are a number of risk factors associated with women’s health and reproductive cycles, including suicide risk during the perinatal, premenstrual, and perimenopausal periods. Suicide is the leading cause of death in perinatal women, with the highest risk being 9-12 months postpartum, yet suicide during pregnancy and the post-partum period is under-researched and most likely underreported (Zagrabbe, 2018).
In general, research has consistently shown that women are more likely to attempt suicide than men yet are less likely to die by suicide than men. This is mostly due to the means of suicide, as men are more likely to use firearms than women (SPRC, 2020). However, during the 9-12-month postpartum period women are likely to choose lethal means. It is also important to note that previous suicide attempt is the greatest risk factor for suicide death in the future. Perinatal mood and anxiety disorders (PMADs) are another risk factor associated with women’s health and suicide. PMADs are considered the number one complication of pregnancy and childbirth, affecting 1 in 7 pregnant and post-partum women and costing approximately $14 billion each year (Luca et al., 2019).
One study found that:
- 1 out of every 19 deaths in pregnant or postpartum women is attributed to suicide.
- 9 to 12 months postpartum may be a time when women are particularly vulnerable and at risk for completing suicide.
- The highest rates of perinatal suicide occurred in women who lived in rural areas.
- Women who completed suicide in the perinatal period were just as likely to have visited primary (non-mental health) care or obstetric care in the preceding month or year as the group of living perinatal women.
- Less than 40% of women who completed suicide in the perinatal period had seen a psychiatrist or primary care provider specifically for mental health issues in the 30 days prior to their death (Grigoriadis et al., 2017).
While psychiatrists regularly screen for suicide, research highlights how important it is to screen perinatal women for suicide in primary care or obstetric offices, as many of the women who go on to complete suicide may never see a psychiatrist.
Suicide Pathway for OB/GYN Settings
While OB/GYNs mostly focus on women’s reproductive health, data show that they are in a unique position to provide suicide care to the patients they serve. There is an increasing need for screening, assessment, and treatment for suicide in the perinatal population, including early identification, identifying potential risk factors (i.e. age, relationship status, race, intent of becoming pregnant, etc.), and red flags related to suicide.
Risk factors for pregnant women:
- Depression, anxiety, or other mental health conditions
- Partner violence
- Unstable or dangerous living environment
- Substance abuse
- Past suicide attempt
Screening
OB/GYNs often provide routine medical services and preventive screenings, and suicide screening should be incorporated into the care pathway for all patients seen by an OB/GYN.
Patient Health Questionnaire-9 (PHQ-9): The PHQ-9 is a self-administered (but can be clinician-administered) screening tool for depression that has a specific question (Question #9) regarding suicide. The PHQ-9 is scored from 0 (not at all) to 3 (nearly every day). The PHQ-9 is shorter than other scales, can be administered in person, by telephone, or self-administered, facilitates diagnosis, provides assessment of symptom severity, is validated in a variety of populations, and can be used in adolescents as young as 12 years old.8 Question #9 specifically asks whether respondents have “thoughts that you would be better off dead or of hurting yourself in some way.” Regardless of the total score, a positive response to question # 9 warrants further risk assessment.
| Severity Levels | PHQ-9 score |
|---|---|
| Normal | 0 - 4 |
| Mild | 5 - 9 |
| Moderate | 10 - 14 |
| Moderate to severe | 15 - 19 |
| Severe | 20 - 27 |
This tool has been validated for its use in primary care settings and can be a critical tool in assisting primary care providers in diagnosing depression and suicide risk and monitoring treatment response.9
- One study found that those who answered “nearly every day” to question 9 on the PHQ-9 had a 4% probability of suicide attempt in the following year, a ten-fold increase compared to .04% of those who answered “not at all.”10
- Another large study found that those who score positive on Question #9 of the PHQ-9 were 5 to 8 times more likely to attempt suicide and 3 to 11 times more likely to die by suicide within 30 days, and were 2 to 4 times more likely to attempt suicide and 2 to 6 times more likely to die by suicide within a year. This increased risk persisted for two years.11
This data shows that suicidal ideation reported on the PHQ-9 is a robust indicator of suicide attempts and deaths, demonstrating the need for providers and healthcare systems to address immediate and sustained risk for suicide in patients who screen positive on the PHQ-9.11
Edinburgh Postnatal Depression Scale (EPDS): As research shows the year post-partum is a particularly vulnerable period for women regarding suicidal ideation, it is important that screening for suicide continue into the post-partum period. OB/GYNs should incorporate screening into the first post-partum visit with a patient and other future visits as needed. While generally intended for use within pediatric settings, OB/GYNs can use the Edinburgh Postnatal Depression Scale to screen women for postnatal depression. The EDPS takes less than 5 minutes to complete and can be self-administered. The EDPS contains a question on suicide (Question #10) that specifically asks about the thought of harming oneself.
- All patients scoring 9 or more should be further assessed
- All patients who score 1 or more on question #10, despite total score, should be further assessed.
Assessment
Assessment and follow-up after screening for suicide risk among perinatal women and all patients is crucial. When screening results in any indication of suicidal ideation, further assessment can be completed using an evidence-based assessment tool.
Columbia-Suicide Severity Rating Scale (C-SSRS): This tool can be used to both screen and assess suicide risk. The C-SSRS is utilized to identify whether the patient has thought about suicide, has taken action or plans to take action, or whether they attempted suicide or plan to attempt suicide. The questionnaire begins with two questions about passive or active suicidal ideations, leading to further follow up questions based on positive responses to gauge severity. Based on the severity, resources are available with interventions for responding to the C-SSRS. This tool has an expansive evidence base, and is supported by SAMHSA, the CDC, the FDA, the NIH, the WHO, and many others. The tool is scored as Low, Moderate or High risk, depending on positive answers. The most concerning answers include: a recent (past month) “yes” to question 4 or 5 (shown below) on ideation severity and/or any recent (past 3 months) behavior.
- An extra benefit of the C-SSRS is built-in triage guidelines. This link contains Clinical Triage Guidelines using the C-SSRS.
- While the C-SSRS is unique in that it can be used by healthcare professionals, as well as friends, families, and individuals in the community, training staff to use the C-SSRS and all screening tools is important in increasing their comfort level and sense of competence. Training resources both online or in-person
|
Ask questions that are in bold and underlined. |
Past month |
|
|---|---|---|
|
Ask Questions 1 and 2 |
YES |
NO |
|
1) Have you wished you were dead or wished you could go to sleep and not wake up? |
|
|
|
2) Have you had any actual thoughts of killing yourself? |
|
|
|
If YES to 2, ask questions 3, 4, 5, and 6. If NO to 2, go directly to question 6. |
||
|
3) Have you been thinking about how you might do this? e.g. “I thought about taking an overdose but I never made a specific plan as to when where or how I would actually do it….and I would never go through with it.” |
|
|
|
4) Have you had these thoughts and had some intention of acting on them? as opposed to “I have the thoughts but I definitely will not do anything about them.” |
|
|
|
5) Have you started to work out or worked out the details of how to kill yourself? Do you intend to carry out this plan? |
|
|
|
6) Have you ever done anything, started to do anything, or prepared to do anything to end your life? Examples: Collected pills, obtained a gun, gave away valuables, wrote a will or suicide note, took out pills but didn’t swallow any, held a gun but changed your mind or it was grabbed from your hand, went to the roof but didn’t jump; or actually took pills, tried to shoot yourself, cut yourself, tried to hang yourself, etc.
If YES, ask: Was this within the past 3 months? |
Lifetime |
|
|
|
|
|
|
Past 3 Months |
||
|
|
|
|
Response Protocol to C-SSRS Screening
Item 1 - YELLOW - Behavioral Health Referral
Item 2 - YELLOW - Behavioral Health Referral
Item 3 - ORANGE - Behavior Health Consult (Psychiatric Nurse/Social Worker) and consider Patient Safety Precautions
Item 4 - RED - Behavioral Health Consultation and Patient Safety Precautions
Item 5 - ORANGE - Behavior Health Consult (Psychiatric Nurse/Social Worker) and consider Patient Safety Precautions
Item 6 - 3 months ago or less - RED - Behavioral Health Consultation and Patient Safety Precautions
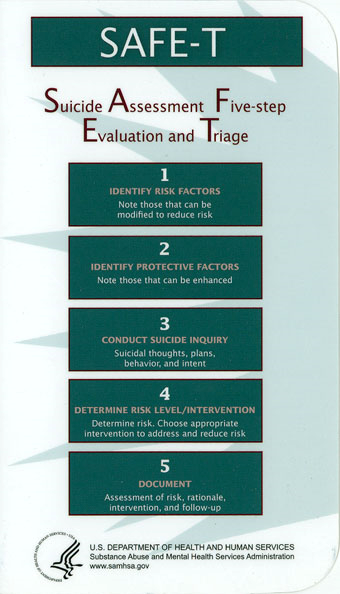
Suicide Assessment Five-Step Evaluation and Triage (SAFE-T): Typically found in the form of the SAFE-T Protocol Card, SAFE-T is a 5-step suicide assessment protocol used to address a patient’s level of suicide risk and suggest appropriate interventions. SAFE-T Quick Guide for Clinicians, a detailed guide for the 5 steps below, with specific language and scripts.
CSSRS with Safe-T Protocol: SAMSHA created a protocol for the SAFE-T assessment that has embedded CSSR-S questions.
Step 1: Identify Risk Factors |
|||
|
C-SSRS Suicidal Ideation Severity |
Month |
||
|
|
||
|
|
||
|
|
||
|
|
||
|
|
||
|
C-SSRS Suicidal Behavior: "Have you ever done anything, started to do anything, or prepared to do anything to end your life?” Examples: Collected pills, obtained a gun, gave away valuables, wrote a will or suicide note, took out pills but didn’t swallow any, held a gun but changed your mind or it was grabbed from your hand, went to the roof but didn’t jump; or actually took pills, tried to shoot yourself, cut yourself, tried to hang yourself, etc. If “YES” Was it within the past 3 months? |
Lifetime |
||
|
|
|||
|
Past 3 Months |
|||
|
|
|||
|
Activating Events: □ Recent losses or other significant negative event(s) (legal, financial, relationship, etc.) Treatment History: □ Previous psychiatric diagnosis and treatments Other: □ ___________________ |
Clinical Status: □ Hopelessness
|
||
|
□ Access to lethal methods: Ask specifically about presence or absence of a firearm in the home or ease of accessing |
|||
Step 2: Identify Protective Factors (Protective factors may not counteract significant acute suicide risk factors) |
|||
|
Internal: □ Fear of death or dying due to pain and suffering □ Identifies reasons for living □ ___________________ □ ___________________ |
External: □ Belief that suicide is immoral; high spirituality □ Responsibility to family or others; living with family □ Supportive social network of family or friends □ Engaged in work or school |
||
Step 3: Specific questioning about Thoughts, Plans, and Suicidal Intent – (see Step 1 for Ideation Severity and Behavior) |
|||
|
C-SSRS Suicidal Ideation Intensity (with respect to the most severe ideation 1-5 identified above) |
Month |
||
|
Frequency How many times have you had these thoughts? (1) Less than once a week (2) Once a week (3) 2-5 times in week (4) Daily or almost daily (5) Many times each day |
|
||
|
Duration When you have the thoughts how long do they last? |
|
||
|
Controllability Could/can you stop thinking about killing yourself or wanting to die if you want to? |
|
||
|
Deterrents Are there things - anyone or anything (e.g., family, religion, pain of death) - that stopped you from wanting to die or acting on thoughts of suicide? (1) Deterrents definitely stopped you from attempting suicide |
|
||
|
Reasons for Ideation What sort of reasons did you have for thinking about wanting to die or killing yourself? Was it to end the pain or stop the way you were feeling (in other words you couldn’t go on living with this pain or how you were feeling) or was it to get attention, revenge or a reaction from others? Or both? (1) Completely to get attention, revenge or a reaction from others |
|||
|
Total Score |
|
||
Step 4: Guidelines to Determine Level of Risk and Develop Interventions to LOWER Risk Level“The estimation of suicide risk, at the culmination of the suicide assessment, is the quintessential clinical judgment, since no study has identified one specific risk factor or set of risk factors as specifically predictive of suicide or other suicidal behavior.” |
||
|---|---|---|
|
RISK STRATIFICATION |
TRIAGE |
|
|
High Suicide Risk Suicidal ideation with intent or intent with plan in past month (C-SSRS Suicidal Ideation #4 or #5) Or Suicidal behavior within past 3 months (C-SSRS Suicidal Behavior) |
□ Initiate local psychiatric admission process □ Stay with patient until transfer to higher level of care is complete
|
|
|
Moderate Suicide Risk Suicidal ideation with method, WITHOUT plan, intent or behavior in past month (C-SSRS Suicidal Ideation #3) Or Suicidal behavior more than 3 months ago (C-SSRS Suicidal Behavior Lifetime) Or Multiple risk factors and few protective factors |
□ Directly address suicide risk, implementing suicide prevention strategies □ Develop Safety Plan
|
|
|
|
Low Suicide Risk Wish to die or Suicidal Ideation WITHOUT method, intent, plan or behavior (C-SSRS Suicidal Ideation #1 or #2) Or Modifiable risk factors and strong protective factors Or □ No reported history of Suicidal Ideation or Behavior |
□ Discretionary Outpatient Referral |
Step 5: Documentation |
||
|
Risk Level [ ] High Suicide Risk |
||
|
Clinical Note:
|
||
Intervention
Patient Education on Suicide Care Management: Script that providers can use to educate patients who are at risk for suicide when they are placed on a pathway to care or suicide treatment care management plan.
Lethal Means Restriction: Anyone who is identified with any level of suicide risk, from mild to severe, should be asked about access to lethal means.
Women who completed perinatal suicide were more likely to do so by lethal methods, like hanging, jumping, or falling, compared to women who completed suicide outside of the perinatal period (Zagrabbe, 2018).
Removing access to lethal means for individuals at risk for suicide should be a top priority, as research shows that over 50% of suicides are completed using a firearms.12 In Montana, firearms were used in 63% of suicides in 2016, though less among women.13 Providers and patients should discuss and monitor other lethal means as well, such as access to materials for hanging/suffocation (belts, ropes, or other items) or large quantities of high-risk medications.
Counseling on Access to Lethal Means (CALM): CALM is a workshop that helps providers identify patients who would benefit from lethal means counseling strategies, ask about access to lethal means, and work with patients and their family to reduce access.14 More information and guidance about which patients need counseling on access to lethal means
- Workshop
- For Clinicians: Sample language and steps, goals, and things to consider when talking with patients about reducing access to lethal means.
- What Clients and Families Need to Know
- Basics of Firearms
- Firearms Laws Relevant to Lethal Means Counseling
Suicide Safety Planning: Much like action plans for physical illnesses, creating a Suicide Safety Plan can be useful for patients to refer to during moments of distress. Suicide Safety Planning is evidence-based and can help patients manage suicidal thoughts and reduce emergency rooms visits. Safety Plans are created by the patient in conjunction with a provider. Safety Plans include identifying triggers and warning signs, specific activities that can steer the patient from suicidal thoughts, contacts to be used during times of distress (community, professional, and emergency), etc.
- Training for staff on how to create a safety plan
- Suicide Safety Planning Quick Guide
- Safety Plan pdf
Other Resources
- Suicide Safer Care webinar
- Now Matters Now: Now Matters Now is an online resource center for providers as well as individuals experiencing suicidal ideation. The website contains training for both patients and providers (meditation, safety planning, curbing suicidal thoughts, etc.) and a number of videos containing personal stories, skills, and resources for support.
- Post-partum Support International Montana Resource Page: This resource contains Support Coordinators and their contact information, emergency resources, support groups, and events.
References:
- Zagrabbe, 2018. https://womensmentalhealth.org/posts/perinatal-suicide-highest-risk-occurs-at-9-to-12-months-postpartum/
- SPRC, 2020. https://sprc.org/about-suicide/scope-of-the-problem/
- Luca et al, 2019. https://www.mathematica.org/our-publications-and-findings/publications/societal-costs-of-untreated-perinatal-mood-and-anxiety-disorders-in-the-united-states
- Grigoriadis S, Wilton AS, Kurdayak PA et al. Perinatal suicide in Ontario, Canada: a 15 year population-based study. CMAJ 2017; Aug 28;189(34):E1085-1092.

