Measles (Rubeola)

Measles Cases and Outbreaks
View the Measles Cases and Outbreaks.
Jurisdiction-Specific Exposure Locations
For information about measles exposure locations in Montana, please view the local health department websites linked here: Cascade, Lewis and Clark, Flathead, Yellowstone, Hill, and Gallatin.
Jurisdiction-Specific Vaccine Recommendations for Residents and Visitors
-
Gallatin County: On December 4, 2025, Gallatin City-County Health Department issued an accelerated administration schedule consideration for Measles, Mumps, and Rubella (MMR) vaccine for all residents and visitors due to recent confirmed cases of measles in the Gallatin community. The considerations include early and accelerated vaccination for children and an additional MMR dose for adults wo have received one dose. More information can be found by visiting the Gallatin City-County Health Department measles page.
Your best protection against measles is vaccination. Talk to your health care provider or county or tribal health department to find where you or your child can get a measles vaccine.
If you are concerned that you have measles or may have been exposed to someone with measles, please contact your county or tribal health department or primary care provider before seeking care, if safe to do so, for instructions about how to avoid exposing others.
Measles activity in states and provinces surrounding Montana can be found on each neighboring jurisdiction’s website:
-
-
Saskatchewan, Canada
-
Alberta, Canada
- British Columbia , Canada
-
-
For MTDPHHS Press Releases related to measles, visit https://dphhs.mt.gov/News/index.
-
For more information on Measles activity in the United States, visit https://www.cdc.gov/measles/data-research/index.html.
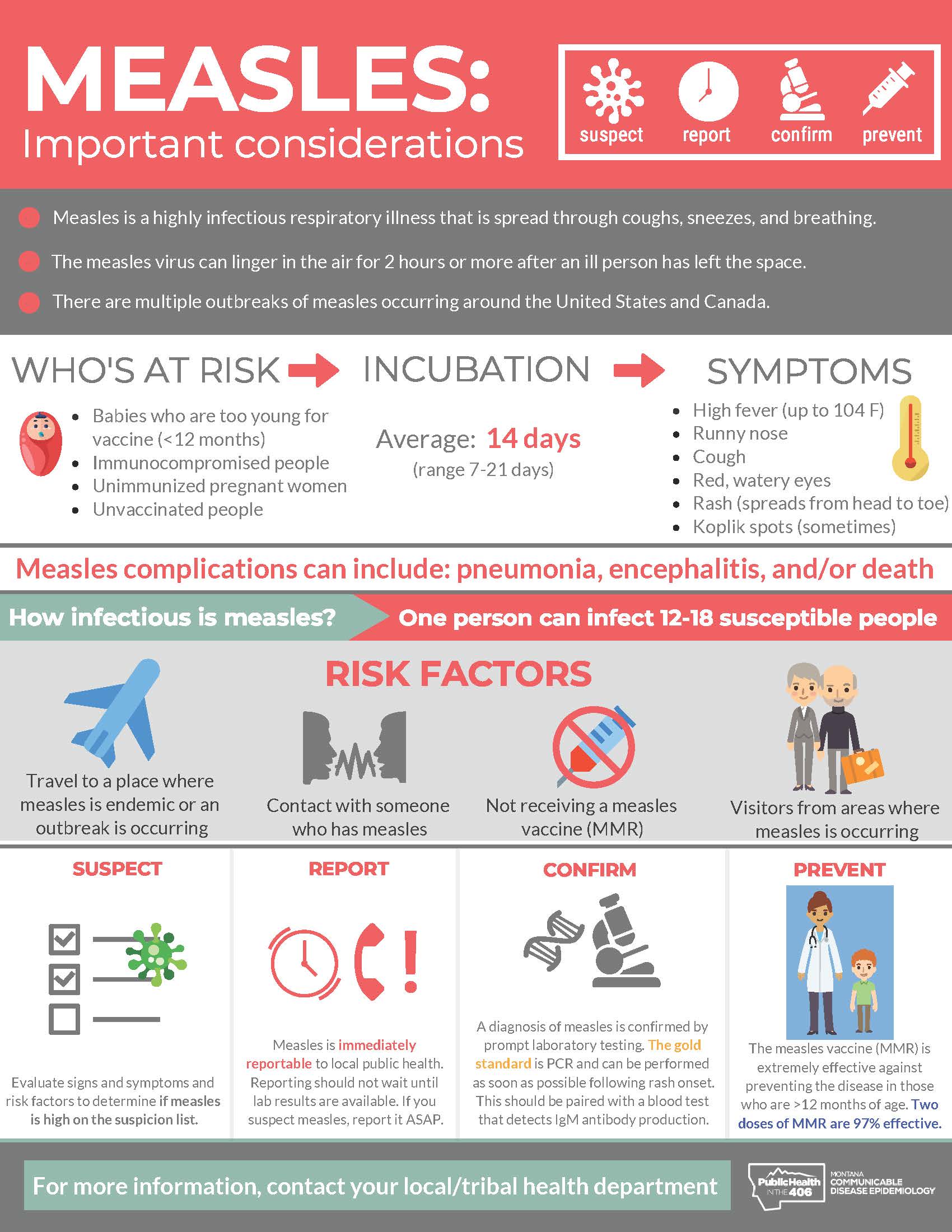
What You Need to Know
Measles is a respiratory disease caused by a virus, and is one of the most contagious of all infectious diseases. Measles can cause serious health complications even in previously healthy people. Complications can includee pneumonia, encephalitis (brain inflammation that can cause permanent brain damage), and death. People most at risk of severe complications include children younger than 5 years old, adults older than 20, pregnant women, and immunocompromised persons. In the United States in 2025, 23% of all reported measles cases under 5 years old have been hospitalized.
Measles is a highly contagious virus that lives in the nose and throat mucus of an infected person. The virus spreads through the air when an infected person coughs or sneezes. It is so contagious that if one person has it, 9 out of 10 people around them will also become infected if they are not protected (see "Prevent Against Measles" tab below).
-
You can get measles just by being in a room where a person with measles has been, even up to two hours after that person has left.
-
An infected person can spread measles to others even before they develop symptoms—from four days before they develop the measles rash through four days after the development of the rash.
-
For more information on transmission, see CDC: Measles transmission.
- 7-14 Days After Becoming Infected
- Symptoms of measles will usually appear 7-14 days after becoming infected with the virus, but can sometimes take up to 21 days to appear.
- Symptoms of measles infection include:
- High fever (may spike to more than 104°F)
- Cough
- Runny nose (coryza)
- Red, watery eyes (conjunctivitis)
- 2-3 Days After Symptom Onset: Koplik Spots
- Tiny white spots, called "Koplik Spots", may appear inside the mouth 2-3 days after initial symptoms (listed above) begin.

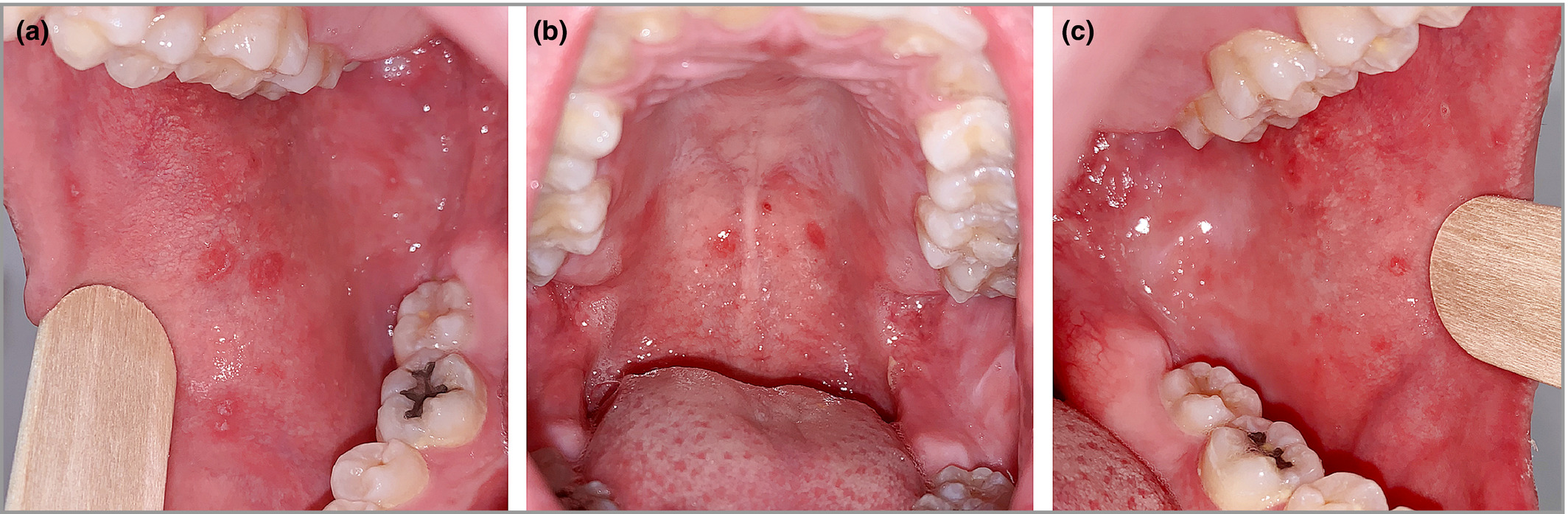
- 3-5 Days After Symptom Onset: Measles Rash
- The measles rash will appear 3-5 days after initial symptoms (listed above) begin.
- The rash will begin on the face at the hairline and then spread downward to the neck, abdomen, arms, legs, and feet.
- The rash will appear to be flat red spots. Small raised bumps may also appear on top of the flat red spots.
- The spots may become joined together as they spread from the head to the rest of the body.


-
If you are concerned that you may have been exposed to someone with measles, please contact your county or tribal health department or primary care provider.
-
Consider staying home until you know more about your risk of becoming ill. If you become ill, please contact your healthcare provider prior to presenting at the healthcare facility, if safe to do so.
-
If you’re not already protected, get a measles vaccine.
-
If given within 72 hours of initial exposure, the MMR vaccine offers protection and lessens the severity of disease.
-
Except in healthcare settings, unvaccinated people who receive their first dose of MMR vaccine within 72 hours after exposure may return immediately to childcare, school, or work.
-
-
Unsure if you’re protected against measles? Check with your healthcare provider or local or tribal health department to request a vaccine record. You can also request a record through Montana’s Immunization Information System by clicking here: https://dphhs.mt.gov/publichealth/immunization/copyofimmunizationrecord
Measles can be serious in all age groups. However, there are several groups that are more likely to suffer from measles complications, including:
-
Children younger than 5 years of age
-
Adults older than 20 years of age
-
Pregnant women
-
People with weakened immune systems, such as from leukemia or HIV infection
Measles can cause serious health complications, such as pneumonia (infection of the lungs), encephalitis (swelling of the brain), and even death.
-
Hospitalization. About 1 in 5 unvaccinated people in the U.S. who get measles is hospitalized due to their illness.
-
Pneumonia. As many as 1 out of every 20 children with measles gets pneumonia, the most common cause of death from measles in young children.
-
Encephalitis. About 1 child out of every 1,000 who get measles will develop encephalitis (swelling of the brain). This can lead to convulsions and leave the child deaf or with intellectual disability.
-
Death. Nearly 1 to 3 of every 1,000 children who become infected with measles will die from respiratory and neurologic complications.
-
Complications during pregnancy. If you are pregnant and have not had the MMR vaccine, measles may cause birth prematurely, or have a low-birth-weight baby.
For more information on complications, see: CDC: Measles Symptoms and Complications.
-
The best protection against measles is vaccination.
-
Talk to your health care provider or local public health department to find where you or your child can get a measles vaccine.
-
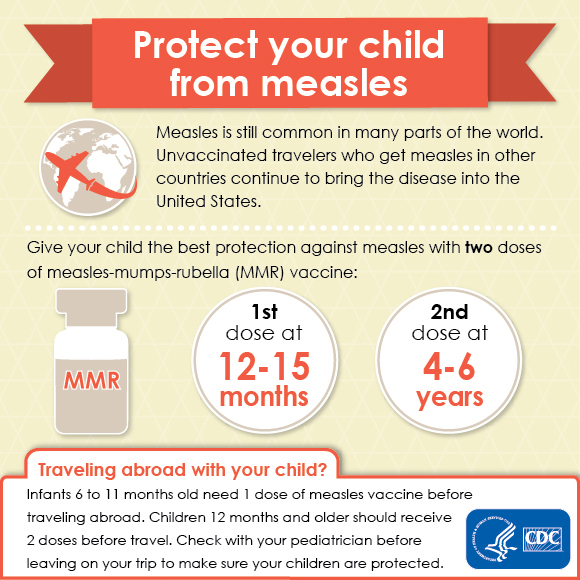
Parents should make sure their children are protected against measles with two doses of MMR vaccine–the first dose at 12 through 15 months of age and the second dose 4 through 6 years of age.
-
The MMR vaccine provides long-lasting protection against all strains of measles. Make sure you’re up to date on MMR and other vaccinations, such as for tetanus and polio.
-
For more information on vaccination, see: Montana Immunization Program and CDC: Measles vaccination.
Multiple measles outbreaks are occurring throughout the United States and internationally.
It is recommended that international travelers and travelers to areas where measles outbreaks are occurring are up to date with measles vaccination. Talk to your doctor about the MMR vaccine for you and your family if you are traveling to an area with known measles transmission.
Information for Healthcare Professionals and Public Health Departments
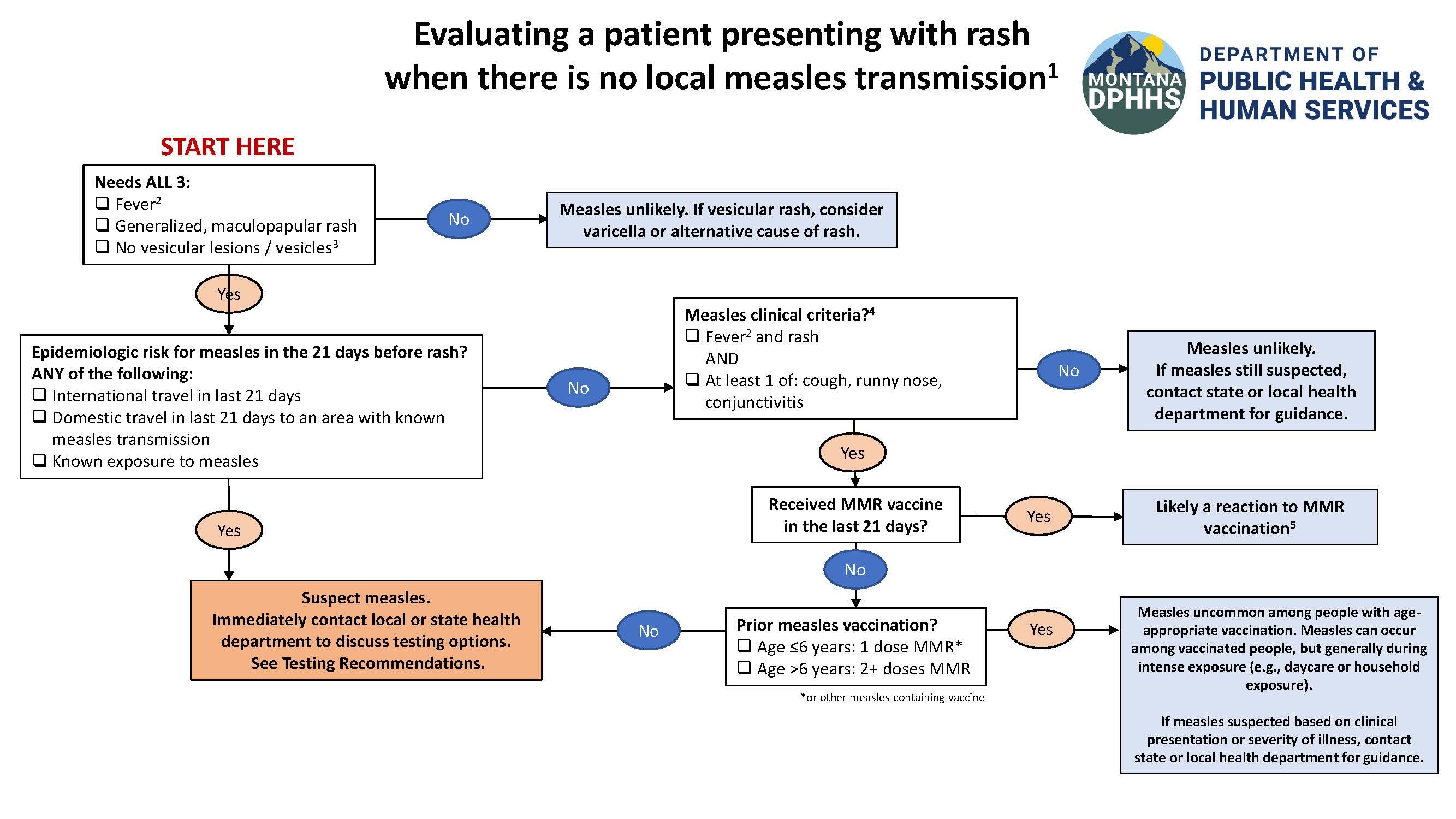
Click the Flowchart Above to View a Larger Version
-
Consider measles in patients presenting with febrile rash illness and clinically compatible measles symptoms (cough, coryza, and conjunctivitis), and ask patients about any recent travel within Montana, the United States, and internationally.
-
If you suspect that your patient may have measles, follow the steps below:
-
If safe to do so, immediately place a mask on the patient and isolate the patient in a room with a closed door (a negative pressure room should be used if available in your facility). For more information on patient placement, see the tab below titled "Patient Placement".
-
Follow standard and airborne precautions.
-
Immediately report the suspected case to your county or tribal health department. If your county or tribal health department are not available, contact Montana Communicable Disease Epidemiology at (406) 444-0273.
-
Only allow health care workers with presumptive evidence of measles immunity to attend the patient. Any person attending to the patient should use a fit-tested N-95 mask, regardless of immunity status. Regardless of presumptive immunity status, all healthcare staff entering the room of the patient should use respiratory protection consistent with airborne control precautions. Presumptive evidence of measles immunity for healthcare workers (one of the following): documentation of two doses of measles-containing vaccine, laboratory evidence of immunity (positive IgG), laboratory evidence of disease, or birth before 1957. Consider vaccinating healthcare workers born before 1957 who do not have other evidence of immunity to measles. Self-reported doses and a history of vaccination provided by a parent or other caregiver, or a clinical diagnosis of measles, should not be accepted.
-
Obtain specimens for testing from patients with suspected measles, including viral specimens for genotyping, which can help determine the source of the virus. Coordinate with your local health department with questions about submitting specimens for testing. Proper PPE should be worn during specimen collection. Review Montana Public Health Laboratory Guidance on Measles Testing and CDC: Measles, Mumps, Rubella, and Varicella Testing.
-
Contact infection control if available at your facility.
-
After the patient leaves the room, it should remain vacant for the appropriate time (at least 2 hours) to allow for 99.9% of airborne-contaminant removal. (See Appendix B, Table B.1.: Air changes/hour and time required for airborne-contaminant removal by efficiency.)
-
Immediately place patients in an airborne infection isolation room (AIIR).
-
An AIIR should meet current standards including:
-
Providing at least six (existing facility) or 12 (new construction/renovation) air changes per hour
-
Directing exhaust of air to the outside
-
If an AIIR does not directly exhaust to the outside, the air may be returned to the air handling system or adjacent spaces if all air is directed through HEPA filters
-
-
When an AIIR is in use for a patient on Airborne Precautions, monitor air pressure daily with visual indicators (e.g., smoke tubes, flutter strips), regardless of the presence of differential pressure sensing devices (e.g., manometers).
-
Keep the AIIR door closed when not required for entry and exit.
-
Patients with measles should remain in Airborne Precautions for 4 days after the onset of rash (with onset of rash considered to be Day 0).
-
Immunocompromised patients with measles should remain in Airborne Precautions for the duration of illness due to prolonged virus shedding.
-
-
-
If an AIIR is not available, transfer the patient as soon as possible to a facility where an AIIR is available.
-
Pending transfer, place the masked patient in a private room with the door closed, if safe to do so. If feasible, the patient should continue to wear the mask for the duration of time spent in the non-AIIR room.
-
Preferably, the patient should be placed in a room where the exhaust is recirculated with high-efficiency particulate air (HEPA) filtration.
-
After the patient leaves the room, it should remain vacant for the appropriate time (at least 2 hours) to allow for 99.9% of airborne-contaminant removal. (See Appendix B, Table B.1.: Air changes/hour and time required for airborne-contaminant removal by efficiency.)
-
-
ACIP recommends that people who don't have presumptive evidence of immunity to measles, mumps, and rubella should get vaccinated against these diseases.
Presumptive evidence of immunity can be established in any of the following ways:
-
Written documentation of adequate vaccines for measles, mumps, and rubella
-
Laboratory evidence of immunity
-
Laboratory confirmation of disease
-
Birth before 1957
Although birth before 1957 is considered acceptable evidence of immunity for healthcare personnel in routine circumstances, healthcare facilities should consider vaccinating healthcare personnel born before 1957 who lack laboratory evidence of immunity or laboratory confirmation of disease.
Healthcare providers should not accept verbal reports of vaccination without written documentation as presumptive evidence of immunity.
Measles Vaccination for Specific Groups
Routine Recommendations
CDC recommends children should routinely get 2 doses of MMR vaccine:
-
First dose at age 12 through 15 months
-
Second dose at age 4 through 6 years (before school entry)
This can be administered as MMR or MMRV vaccine. Children can receive the second dose of MMR vaccine earlier than 4 through 6 years (as long as it is at least 28 days after the first dose). A second dose of MMRV vaccine can be given 3 months after the first dose up to 12 years of age.
CDC recommends that separate MMR and varicella vaccines be given for the first dose in children aged 12–47 months; however, MMRV may be used if parents or caregivers express a preference.
Adults and teens should also be up to date on MMR vaccinations with either 1 or 2 doses (depending on risk factors); unless they have other presumptive evidence of immunity to measles, mumps, and rubella. MMR vaccination is especially important for healthcare professionals, international travelers, and other specific groups.
One dose of MMR vaccine, or other presumptive evidence of immunity, is sufficient for most adults. Providers generally do not need to actively screen adult patients for measles immunity in non-outbreak areas in the United States. After vaccination, it is also not necessary to test patients for antibodies to confirm immunity. There is no recommendation for a catch-up program among adults for a second dose of MMR (e.g., people born before 1989 or otherwise).
People exposed to measles who cannot readily show that they have adequate presumptive evidence of immunity against measles should be offered post-exposure prophylaxis (PEP). Public health officials can help identify eligible persons, assess any contraindications, and weigh benefits.
There are two types of PEP for measles. To potentially provide protection or modify the clinical course of disease among susceptible persons, administer one of these:
-
MMR vaccine, if administered within 72 hours of initial measles exposure.
-
Immunoglobulin (IG), if administered within 6 days of exposure. The recommended dose for intramuscular immunoglobulin (IMIG) is 0.5mL/kg, regardless of the contact’s immune status.
-
If administering IG, infection control precautions such as PPE use and implementation of transmission-based precautions should be adhered to prevent additional exposures.
-
Don't administer MMR vaccine and IG simultaneously. This practice invalidates the vaccine.
More information on measles PEP can be found here: https://www.cdc.gov/mmwr/preview/mmwrhtml/rr6204a1.htm
This document provides general information on the Montana Human Rights Act provision (§ 49-2-312, MCA) that bars discrimination on the basis of vaccination status as it relates to measures that might be taken by local health departments, schools, child care facilities, and health care facilities to control the spread of measles. The information contained in this document does not, and is not intended to, constitute legal advice. Readers of this document are strongly encouraged to consult with their attorney to obtain advice with respect to whether a particular policy, practice, or procedure is compliant with the Montana Human Rights Act (§ 49-2-312, MCA), or whether such action may constitute a prohibited act of discrimination.
-
Video: Clinical Overview of Measles: Diagnosis, Laboratory Testing, and Outbreak Response
-
Earn Continuing Education (CE) Credits for This Course
-
To receive continuing education (CE) for this course, Clinical Overview of Measles: Diagnosis, Laboratory Testing, and Outbreak Response (Web on Demand) - WD4728, please visit CDC TRAIN and search for the course in the Course Catalog. Then, follow the steps below.
-
Register for and complete the course.
-
Pass the post-assessment with a percentage of 80%.
-
Complete the evaluation.
-
-
-
Visit Your Learning to access your certificates and transcript.
"Think Measles" Infographic by Project Firstline and the American Academy of Pediatrics
-
-
Healthcare Settings: Places, where healthcare is delivered, include but are not limited to, acute care facilities, long-term acute-care facilities, nursing homes, home healthcare, vehicles where healthcare is delivered (e.g., mobile clinics), and outpatient facilities, such as dialysis centers, physician offices, dental offices, and others.
-
Healthcare Personnel (HCP): HCP refers to all paid and unpaid persons serving in healthcare settings who have the potential for direct or indirect exposure to patients or infectious materials, including body substances (e.g., blood, tissue, and specific body fluids); contaminated medical supplies, devices, and equipment; contaminated environmental surfaces; or contaminated air. These HCP include, but are not limited to, emergency medical service personnel, nurses, nursing assistants, physicians, technicians, therapists, phlebotomists, pharmacists, students and trainees, contractual staff not employed by the healthcare facility, and persons not directly involved in patient care, but who could be exposed to infectious agents that can be transmitted in the healthcare setting (e.g., clerical, dietary, environmental services, laundry, security, engineering and facilities management, administrative, billing, and volunteer personnel).
-
Unprotected Exposure for HCP: HCP exposures to measles in a healthcare setting include spending any time while unprotected (i.e., not wearing recommended respiratory protection):
-
In a shared space with an infectious measles patient at the same time, OR
-
In a shared air space vacated by an infectious measles patient within the prior 2 hours
-
-
Shared Air Space: Smaller spaces, such as the patient compartment of an ambulance, single patient room, or a clinic waiting area, are shared air spaces. Different areas in larger spaces or rooms that share a common air handling system, such as a large emergency department with patient waiting, triage, HCP work areas, or multiple individual patient rooms that share a common unfiltered air source, are also shared airspaces.
-
Source Control: Use of respirators or well-fitting facemask or cloth masks to cover a person’s mouth and nose to prevent spread of respiratory secretions when breathing, talking, sneezing or coughing.
-
High-Risk Group for Severe Illness and Complications: Severely immunocompromised persons, infants too young to be vaccinated, and pregnant women who do not have presumptive evidence of measles immunity are persons considered to be in a high-risk group for severe illness and complications from measles.